Prolapse surgery need not automatically mean hysterectomy
Modern hysteropexy techniques for pelvic organ prolapse (POP) have been around for nearly two decades and have built a solid track record of improving function and patient quality-of-life.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
While the less-invasive hysteropexy is not advisable for every patient, it is important that clinicians consider it when medically appropriate, that they understand their patient’s goals, and that they provide them with information to make empowered decisions. Specifically, shared decision-making should include considerations of the patient’s wishes with regard to her uterus.
That’s the message from Amy Park, MD, Section Head, Urogynecology and Reconstructive Pelvic Surgery in Cleveland Clinic’s Obstetrics & Gynecology Institute. As well established as hysteropexy is for treatment of POP, it hasn’t yet become standard even though many patients, if given the choice, would prefer to retain their uterus.
“People shouldn’t think that they can't have their prolapse repaired if they really want to retain their uterus,” says Dr. Park. “They can, and they may have better outcomes with hysteropexy.”
Women who wish to avoid hysterectomy report a number of reasons, including a desire to retain fertility; a belief that the uterus affects sexual function; concerns about the risks of hysterectomy; and culture-based attitudes about femininity, identity and/or body image.
Still, an estimated 74,000 hysterectomies are performed each year for prolapse in the United States for a variety of reasons.
Among them is that hysterectomy has a long history as the standard intervention. If it is laid out to a patient as the only option for POP repair, says Dr. Park, there is a risk that patients either may experience post-surgical regrets or simply never get the care they need.
Advertisement
“Sometimes patients will hear from their doctors, ‘You need to have a hysterectomy and prolapse repair.’ If the patient is psychologically or emotionally attached to their uterus, they may not come back in, because they don't want to have their uterus removed.”
While more research may be needed before hysteropexy is included as standard of care for POP, Dr. Park says a number of considerations can help inform clinicians and patients.
Advertisement
Finally, says Dr. Park, “Prolapse is a quality-of-life issue. Our approach at Cleveland Clinic focuses very much on symptoms, to what degree they bother the patient, and how people feel about their uterus. A lot of patients are fine with having a hysterectomy at the time of their prolapse repair. But for those who aren’t, there are lots of options now. Prolapse no longer automatically means that repair automatically equals hysterectomy.”

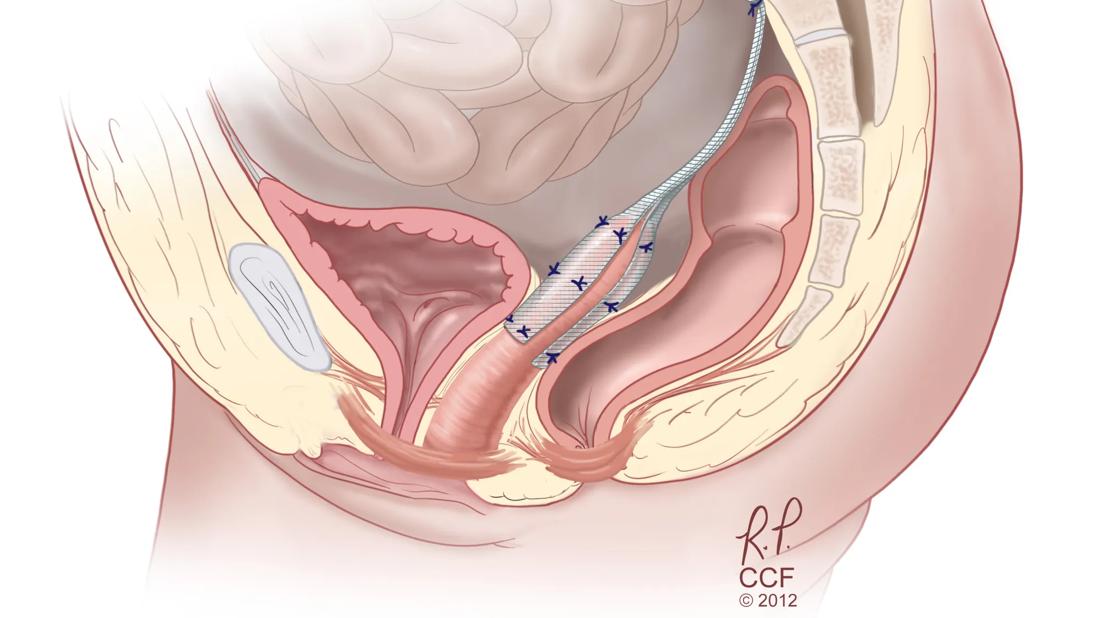
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ba256fa5-b51a-4eae-af8b-29acb1b53c3c/uterine-preservation-during-prolapse-repair-inset)
Advertisement
Advertisement

Specialist teams can improve outcomes and reduce risks

Novel program is life changing for patients and families

Study indicates patients can have confidence about potential outcomes

Addressing the brain-body interplay can help patients achieve better outcomes

New guidelines let the patients steer the process

Uterine transposition cleared the field for radiation therapy

ACOG-informed guidance considers mothers and babies

Artesunate ointment shows promise as a non-surgical alternative