Pioneering surgical tissue recovery work could lead to new and more targeted approaches for treating many forms of hearing loss and vestibular disorders
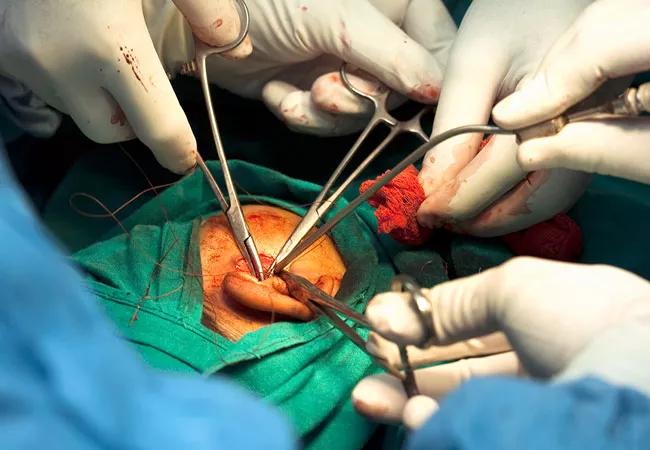
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/72f06ba5-cb83-4364-8eea-120ef3f601a8/22-HNI-3022712-Recvry-Inner-Ear-Tissues-Deceased-Organ-Donors-CQD_650x450_jpg)
22-HNI-3022712-Recvry-Inner-Ear-Tissues-Deceased-Organ-Donors-CQD_650x450
According to the World Health Organization, more than 1.5 billion people worldwide live with hearing loss, a number that could rise to over 2.5 billion by 2030 with the aging population. Current treatment for sensorineural hearing loss is limited to amplification devices or cochlear implants, and in rare cases auditory brainstem implants. But as of now, there is no treatment for loss of inner ear hair cells, the most common underlying pathology associated with both auditory and vestibular disorders. Rehabilitation therapy is the only modality for addressing those.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
More research on the inner ear tissue is needed to identify different therapeutic options, but until now, this has been mostly undertaken in animal models, human fetuses and occasionally adult humans with pathology, such as inner ear or lateral skull base tumors, with access to healthy adult inner ear tissue being scarce. But work from otologist/neurotologist Ksenia A. Aaron, MD at Cleveland Clinic is changing the paradigm. She is currently only one of the few in the world procuring adult human inner ear tissue from deceased organ donors.
Dr. Aaron was an integral part of the team that developed the surgical technique while at Stanford University, and brought the skill to the Cleveland Clinic when she joined in August 2021. Since then, she has worked to establish a workflow process with the nonprofit organ procurement agency, LifeBanc Ohio. When an organ donor becomes available, dedicated teams approach the family and obtain consent for the inner ear tissue donation along with other tissues and organs that are obtained for transplantation. For now, the inner ear tissue is only used for research.
“By looking at the human inner ear we hope to answer a multitude of questions. One is the transcriptional profile of adult human inner ear tissue on a single cell level. What are the single cell transcriptomics that we can see as compared to other animal models like the mouse or non-human primates? To date, healthy human adult inner ear tissue, outside of a utricle, has not been processed on a single-cell level,” Aaron explains.
Advertisement
The translational clinical aim, she explains, is “if we know the underlying landscape then we can do targeted pharmacotherapy to treat those disease processes of hearing loss or vestibular insult instead of just giving everyone steroids in hopes that it might bring the hearing or balance deficit back.”
In two recent papers published in the April 2022 issue of Otology & Neurotology, Dr. Aaron and her colleagues out of Stanford University, highlight the surgical approach to obtaining inner ear tissue and the best practices for selecting appropriate deceased donors.
The former, which was conducted across multiple California centers with the involvement of a regional non-profit federally-funded organ procurement organization, was aimed at developing a surgical approach for rapid and minimally traumatic recovery of fresh inner ear tissue.
The paper details the steps designed to maximize speed and minimize damage, developed by modifying prior procedures: A retro-auricular approach for a trans-canal exposure, approach to the vestibule with extraction of the vestibular end organs, and approach to the cochlea with extraction of the cochlear duct. Optional modifications are also described for obtaining the petrous bone including the 8th cranial nerve attached to the organs.
The second paper describes how the team used immunofluorescence to examine vestibular tissues from 33 ears recovered from 19 organ donors. Five had cardiac death, and the rest brain death. Their analysis showed that the subset of donors with cardiac death, rather than brain death, were optimal for obtaining intact sensory epithelia with hair cells and supporting cells. This was in part because they had shorter resuscitation time, less severe brain insults, and shorter time between pronouncement of death and tissue procurement than for those with brain death.
Advertisement
“The two types of donors have different availability of viable tissue. With cardiac death, it’s more likely that there was enough oxygen and no tissue damage,” she explains.
“The initial challenge was whether we could procure the inner ear quickly. We developed a protocol of doing it in a timely manner where we were able to procure one side of inner ear tissue in under 20 minutes and both sides in under 40 minutes. How you handle the tissues is also very important, since mishandling can affect the quality and the ultimate results based on the question being asked,” Dr. Aaron says.
But the need to work quickly means that logistics can be tricky. “I’ll get called at random hours of the day and I am notified that there is an available organ donor, and the procurement will happen at this time. You have to be ready and available, and sometimes it is not possible as I have clinic or I’m in the operating room.”
But, she’s prepared to jump in as often as possible once the program is fully up and running at Cleveland Clinic. “I’ve applied for several grants. Now it’s just a matter of procuring the tissue and processing it in the lab once the funding is available.”
Advertisement
Advertisement
Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor
Case study illustrates the potential of a dual-subspecialist approach
Evidence-based recommendations for balancing cancer control with quality of life
Study shows no negative impact for individuals with better contralateral ear performance
HNS device offers new solution for those struggling with CPAP
Patient with cerebral palsy undergoes life-saving tumor resection
Specialists are increasingly relying on otolaryngologists for evaluation and treatment of the complex condition
Detailed surgical process uncovers extensive middle ear damage causing severe pain and pressure.