How Cleveland Clinic helped an alliance partner improve on-time starts and more
Cleveland Clinic’s Miller Family Heart & Vascular Institute has maintained a long-standing alliance relationship with the MedStar Heart & Vascular Institute at MedStar Washington Hospital Center, MedStar Union Memorial Hospital and MedStar Southern Maryland Hospital Center in the Baltimore-Washington metro region. This formal relationship offers value through a variety of in-depth services provided by Cleveland Clinic, including the sharing of clinical and quality best practices.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cleveland Clinic also supports its alliance and affiliate colleagues by promoting strategies to assess operational efficiency, resource utilization and standardization to enhance patient throughput and caregiver workflow. An ongoing collaboration between Cleveland Clinic and MedStar Southern Maryland Hospital Center (MSMHC) around one set of these strategies — aimed at reducing late starts and between-procedure turnaround times in the cardiac catheterization lab — initiated an efficiency project at MSMHC in the spring of 2018. That project is the focus of this case study in collaboration.
After identifying cath lab efficiency improvement as a priority, MSMHC leadership recognized that two elements would be crucial to success: the engagement of physician operators, and the leadership of a physician champion to facilitate changes.
Such leadership was obtained early in the cath lab initiative when interventional cardiologist William Suddath, MD, joined MSMHC as Chairman of Cardiology and medical director of the cardiac catheterization lab. Dr. Suddath came from MedStar Washington Hospital Center and was a well-known leader in cardiac care in the region.
To determine opportunities for improvement in cath lab efficiency, Dr. Suddath worked with Director of Cardiology Services Ora Reaves, MBA, RN, and the MSMHC cath lab team to collect data requested by the Cleveland Clinic clinical and continuous improvement teams that were advising MSMHC. Specifically, the requested data were time stamps that provided information on the following:
Advertisement
When the MSMHC team and Cleveland Clinic clinical and continuous improvement teams analyzed the data, they realized that invasive procedures — specifically the first procedures on the daily schedule — were not starting on time. The data further showed that when the first case starts late, all subsequent cases start late as a result, leading to scheduling difficulties and lab utilization inefficiencies that increase the cost of care and result in decreased patient and employee satisfaction.
Additionally, Ora Reaves and her team conducted a manual audit of patient documentation to identify reasons for the case delays so they could be addressed by Dr. Suddath.
The Cleveland Clinic clinical and quality improvement teams recommended that MSMHC address these findings by enforcing a mandatory start time that would hold physicians and cath lab staff accountable for procedures starting on time.
Dr. Suddath was tasked with enforcing the rule — which he calls “bringing the MedStar culture” — among the physician staff, which includes both MedStar physicians and many independent practitioners. The expectation is that all operators are to be present and ready to begin their procedures on time, as is consistent with the MedStar culture of efficiency and accountability, or lose the opportunity to have first-round cases.
The nursing and technical staff are also held accountable for having patients ready on time for their procedures, with this oversight ensured by Ora Reaves.
In July 2018, only 20% of the first cases of the day started on time. Since then, as detailed in the graph below, this percentage has grown to levels approximately three times that rate, reaching 61% in the most recent month reported.
Advertisement
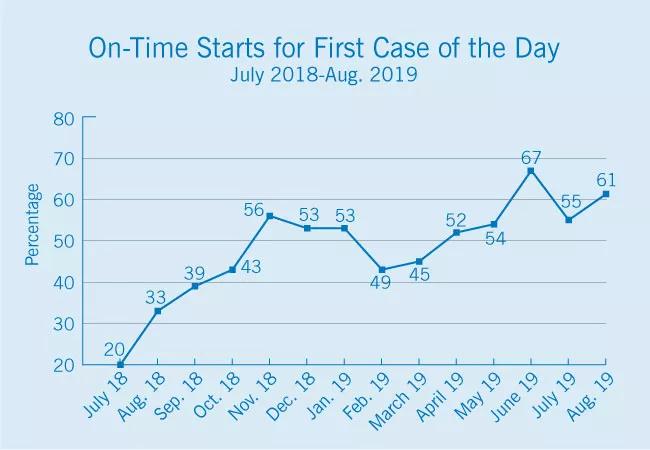
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/88971fd5-2dda-489b-b9b9-e9a0c0cc495e/19-HRT-6510-Chart-1-650x450_jpg)
Another key metric has been room turnover time, or the interval between the “wheels out” time of one case to the “wheels in” time of the next case. The MSMHC team believed their room turnover times, which averaged 68 minutes in July 2018, could be shortened considerably to a target of 25 minutes. Their Cleveland Clinic clinical and quality improvement partners provided recommendations on team members’ roles and responsibilities to help “turn” the cath lab more efficiently between cases. These included process improvements made in pre-procedure documentation, scheduling and room utilization. Ora Reaves was able to come to Cleveland Clinic to observe these processes firsthand in September 2018.
The improvement in cath lab efficiency also resulted in greater work-life balance and employee satisfaction for lab nurses and technicians, which will promote staff retention.
As detailed in the graph below, implementation of these recommendations in mid-2018 was associated with a swift and generally steady decline in room turnover times, with MSMHC achieving times well below its target of 25 minutes in the two most recent months reported.
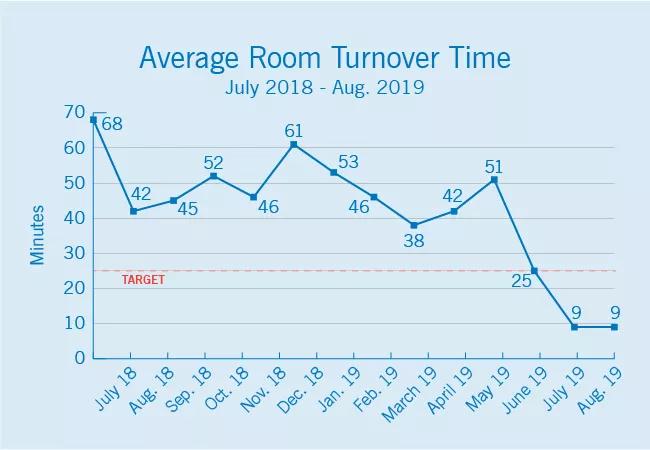
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ea95acfb-bbcd-4fd0-a78a-180b3352d176/19-HRT-6510-Updated-Chart-2-650x450_jpg)
“There are so many people who deserve credit and recognition for these improvements because of their hard work,” says Dr. Suddath.
“This is no small feat,” notes Christopher Bajzer, MD, who is part of the Cleveland Clinic clinical team that works with MSMHC under the alliance partnership. “What the MSMHC team has accomplished in such a short time under Dr. Suddath and Ora’s leadership is truly amazing.”
Advertisement
On the heels of these successes, MSMHC has undertaken other quality improvement efforts, including an initiative to decrease hospital transport time from areas of rural southern Maryland to MSMHC using state of Maryland air transport for patients with suspected ST elevation myocardial infarction (STEMI).
Reduction of STEMI mortality has been a focus of collaboration between Cleveland Clinic and MSMHC. STEMI identification in the field and time to treatment have been identified as opportunities by Dr. Suddath. The aim is to eliminate the use of ground transport to take STEMI patients to the closest hospital, which then often requires transporting them again to MSMHC for cardiac intervention. “Transporting suspected STEMI cases directly to MSMHC by air, with the help of the state, is estimated to cut transport time by 66%,” notes Dr. Suddath.
In support, Cleveland Clinic has supplied its protocols to help effectively triage and transfer patients. “We commend Dr. Suddath and the MSMHC team for undertaking this initiative,” says Dr. Bajzer. “The quicker you get a STEMI patient to treatment, the better the chances of survival and recovery. We look forward to seeing this initiative in action and the effect it will have on MSMHC’s door-to-door-to-balloon time and first medical contact to reperfusion.”
For information on affiliation and alliance opportunities with Cleveland Clinic’s Heart & Vascular Institute, visit clevelandclinic.org/heartaffiliates.
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more