Patient with previous neurological, bone and hematologic involvement presents with hematemesis
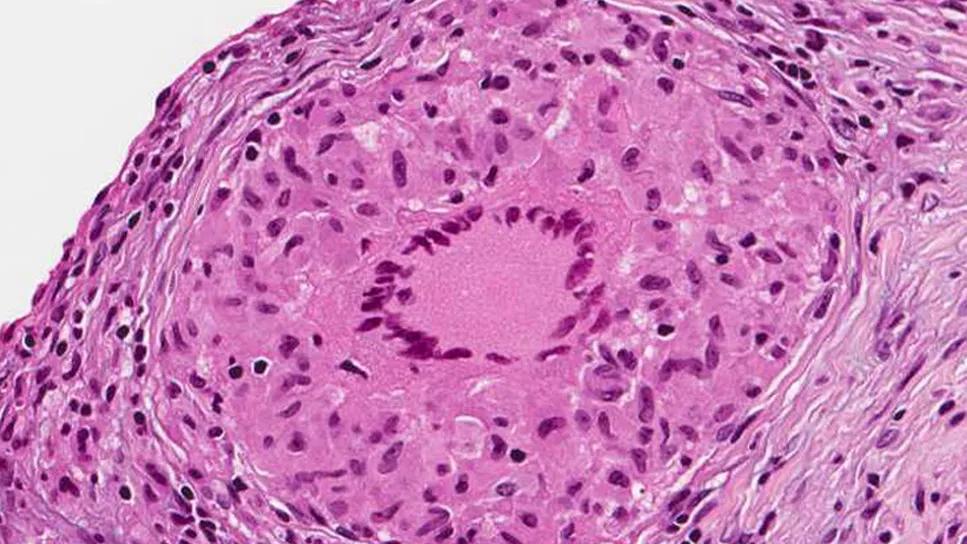
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d02566c1-388f-467d-87c0-1f2b83886dcb/sarcoidosis-granuloma)
Sarcoidosis
A 59-year-old Black male with a past medical history of biopsy-proven sarcoidosis with neurological, bone and hematologic involvement presented with upper gastrointestinal bleeding and acute blood loss anemia. His sarcoidosis had been in remission since 2012 after previous treatment with methotrexate.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
He was admitted to the medical intensive care unit with hematemesis. Esophagogastroduodenoscopy (EGD) showed peptic ulcer disease, and cultures were positive for H. pylori. He continued to rebleed despite multiple embolizations and ultimately required more than 50 units of packed red blood cells transfused over the course of the month. He then underwent a total gastrectomy, splenectomy and esophagojejunal anastomosis with J-tube. Following the procedure, he had another episode of massive bleeding requiring pressors. Interventional radiology angiogram showed active extravasation from the jejunal branch of the superior mesenteric artery. Pathology from the gastrectomy showed numerous well-formed non-necrotizing granulomas involving the entire gastric wall, duodenal tissue, omentum and spleen. Acid-fast bacilli (AFB) and fungal stains were negative.
Watch Juliette Yedimenko, MD, staff in the Department of Rheumatologic and Immunologic Diseases, discuss the case to find out how physicians established the difficult diagnosis of systemic sarcoidosis.
Video content: This video is available to watch online.
View video online (https://www.youtube.com/embed/1vnWJc-3bXQ?feature=oembed)
A Rare Case of Sarcoidosis
“GI tract involvement in sarcoidosis is exceedingly rare, with some studies showing an incidence of symptomatic GI sarcoidosis to be less than one percent,” says Dr. Yedimenko. “Any part of the GI tract can be affected, including the esophagus, stomach, small and large bowel. The diagnosis is difficult to make, as the presence of granulomatous inflammation does not necessarily mean sarcoidosis is responsible for the clinical manifestation, and common GI diseases must be excluded. Treatment is usually high-dose steroids and DMARDs [disease-modifying antirheumatic drugs] such as methotrexate, azathioprine and infliximab. In refractory cases, surgical intervention may be necessary with bowel obstruction, perforation or massive hemorrhage.”
Advertisement
Advertisement
Researching the biological basis for why treatment is or is not effective
Scribing system helps create more face-to-face interactions
A conversation with Leonard Calabrese, DO
The case for continued vigilance, counseling and antivirals
High fevers, diffuse rashes pointed to an unexpected diagnosis
No-cost learning and CME credit are part of this webcast series
Summit broadens understanding of new therapies and disease management
Program empowers users with PsA to take charge of their mental well being