Researchers have developed immunoprofiles for an emerging disease with a mortality rate as high as 27%

Researchers led by Jae Jung, PhD, director of Cleveland Clinic’s Global Center for Pathogen Research & Human Health, have performed the first comprehensive immunoprofiling study of patients with severe fever with thrombocytopenia syndrome (SFTS), an emerging tick-borne disease.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
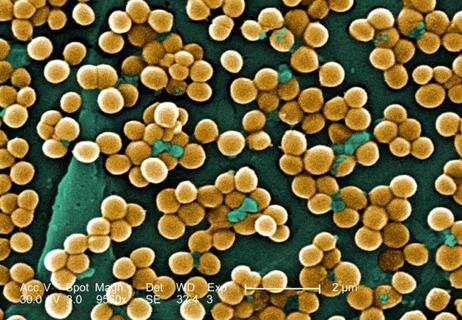
The World Health Organization has classified the virus that causes SFTS—called SFTSV—as among the most likely pathogens to cause widespread epidemics in the future. “The ticks that carry SFTSV have already been found in several states in the United States,” said Dr. Jung, “which signals the growing potential for a domestic outbreak and underscores the need to be doing research now that can help us to get out in front of this threat.”
According to the team’s findings published in mBio, B cells, the immune cells responsible for producing and secreting antibodies, play a crucial role in fatal SFTSV infections. This suggests that targeting B cells—particularly plasma B cells—may help prevent viral replication, although future studies will be necessary.
SFTS is characterized by many various symptoms—including high fever, gastrointestinal complications, low platelet and white blood cell counts, hemorrhage and multi-organ failure—and has a particularly high fatality rate. However, fatality rates vary dramatically by region, ranging anywhere from just over five percent to as high as 27 percent.
“Just for comparison,” Dr. Jung commented, “the mortality rates related to SFTSV infection are much higher than what we’re seeing with SARS-CoV-2 and COVID-19.”
Currently, the biological mechanisms behind these variances in disease symptoms and severity are unknown. In search of these answers, Kyle Jung, a graduate student in Dr. Jung’s lab, analyzed blood samples collected from more than 60 patients in South Korea between 2014 and 2019. These included 40 patients with active SFTSV infection; 11 patients who died from infection; 5 patients who recovered from infection; and 6 healthy controls.
Advertisement
The researchers used precision technologies to uncover the protein and gene expression patterns of individual cells, comparing them across patients in different states of infection.
They found more than 70 inflammatory molecules in patient serum and identified associations between the presence and abundance of certain cytokines and disease severity. Specifically, patient serum samples showed elevated levels of interferon gamma, interleukin 6, caspase 8, SIRT2, CCL7 and CSCL9 in high-risk patients compared to low-risk patients, and increased CCL20, TNFalpha and CX3CL1 in fatal patients.
These findings point to the possible utility of inflammatory biomarkers to help identify which patients infected with the virus are at least and greatest risk for severe disease and death.
Dr. Jung’s team also found that most viral genetic material localized to plasma B cells. Because B cells secrete antibodies, they are one of the main cell types involved in the body’s adaptive immune response. Compared to uninfected plasma B cells, those infected with SFTSV showed signs of reduced interferon signaling, which is a critical precursor to antibody production and secretion.
“Based on our findings, we believe that plasma B cells are the primary host for SFTSV replication,” said Dr. Jung. “Since we found that SFTSV infection suppresses neutralizing antibody production, once viral genetic material makes it into these B cells, the virus is free to replicate, spread and can cause subsequent death.”
Earlier this year, Dr. Jung—who also chairs the Department of Cancer Biology and holds the Betsy B. deWindt Endowed Chair in Cancer Biology—received a $2.8 million grant from the National Institute of Allergy and Infectious Diseases to develop a vaccine against SFTSV. Findings from this study will provide valuable insights for Dr. Jung to build upon in his vaccine study.
Advertisement
Angela Park, PhD, a former lab member of Dr. Jung’s lab at the University of Southern California (USC), and Kyle Jung are first authors on the study, which was supported in part by the National Institutes of Health and made possible by close collaboration with Young-Ki Choi, PhD, from Chungbuk University in South Korea. Dr. Jung joined Lerner Research Institute from USC in August 2020.
Advertisement
Advertisement

Screen patients seeking care for chlamydia, gonorrhea

Lingulectomy removes infection when antibiotics fail

Findings from one of the first published case series
Don't discount this crucial step
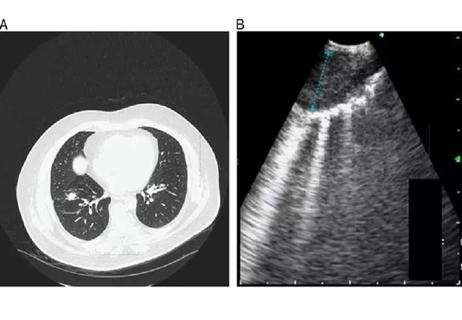
EBUS-TBNA found safe and effective
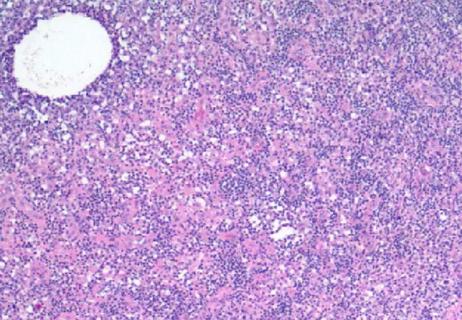
How to spot the rare infection

Not all lung nodules are malignant

An uncommon condition in a 41-year-old man