The tumor's proximity to critical structures made the case challenging

A 15-hour surgery that involves removing a patient’s eye and reconstructing the entire orbit is not common, but surgeons at Cleveland Clinic had experience with such procedures to know exactly what to do when a 39-year-old male patient presented with a constant headache and a protruding eyebrow.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The patient had been diagnosed with a massive stage 4 sinonasal adenocarcinoma involving the orbit of his right eye and the base of his skull. “The challenge with these cancers is the proximity to very critical structures. Because this tumor was involving not only the muscles but the compartment of the orbit, we had to take everything out,” says Eric Lamarre, MD, Section Head for Head and Neck Cancer in Cleveland Clinic’s Department of Otolaryngology-Head & Neck Surgery.
Assisted by a large professional staff, the procedure required the individual expertise of three primary surgeons: Dr. Lamarre, along with Troy Woodard, MD, Section Head of Rhinology, Sinus & Skull Base Surgery at Cleveland Clinic and Pablo Recinos, MD, of the Brain Tumor and Neuro-Oncology Center.
Dr. Recinos worked on the tumor from above by separating it from the brain and helped Dr. Lamarre take the eye and tumor out. Dr. Woodard removed the residual tumor through the patient’s nose.
Dr. Lamarre then performed the reconstructive phase of the surgery, using tissue taken from the patient’s thigh. “You have to seal all the compartments. You can’t have brain fluid communicating with the nose or orbital socket. So, I put in a graft to reconstruct where the eye came out to seal the brain from the orbital socket from the nose,” he explains.
Sinus cancers are fairly rare, but because Cleveland Clinic is a tertiary referral center, Dr. Lamarre sees between six and twelve such cases a year and has performed several of these extended surgeries. “We do a lot of these as a group. Patients come from all over the world,” he notes.
Advertisement
Dr. Lamarre is also a co-author, along with Raj Sindwani, MD, also of the Cleveland Clinic Department of Otolaryngology-Head & Neck Surgery, of the International consensus statement on allergy and rhinology: Sinonasal tumors, published in September 2023. Several of their prior papers served as part of the document’s broad evidence base.
As is the case with most sinonasal tumors, the patient’s diagnosis had been delayed both for clinical and practical reasons. “Sinuses are basically empty spaces of air, so if you have a cancer there it typically takes a while for it to cause symptoms, once it starts to invade other structures,” Dr. Lamarre says.
At the time his symptoms began to appear, the patient had been very busy preparing to open a new business. There were delays, and he attributed his worsening headaches to stress. It wasn’t until a friend commented that his eye looked swollen that the patient looked in a mirror and noticed that his right eyebrow was protruding and he’d been rubbing his eye because it hurt.
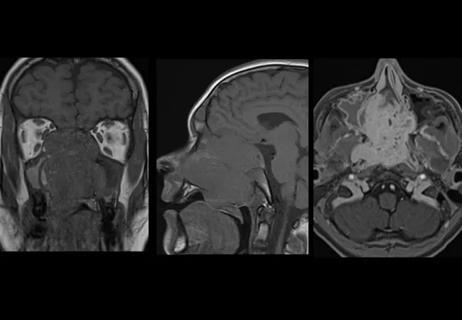
Finally, an MRI showed the massive tumor. The patient first saw Dr. Woodard, who did the biopsy and made the diagnosis.
“We do these procedures fairly seamlessly,” explains Dr. Lamarre. “Our excellent team of surgeons, surgical technologists and nurses have experience managing these cases. We also collaborate with caregivers from a variety of disciplines, including medical and radiation oncologists. This collaborative spirit is deeply ingrained in Cleveland Clinic and allows us to tackle highly complex cancers.”
Advertisement
Today, the patient is doing fine with one eye and comes back to see Dr. Lamarre just once a year for checkups.
The socket where his right eye was is now covered by the grafted skin. “You can use a prosthesis but many patients tend not to because it just remains stationary,” Dr. Lamarre says.
The patient could also wear a patch over the graft if he wanted to, but he chooses not to. “It doesn’t slow him down from a functional standpoint. He’s able to drive and do what he wants. Despite this experience, he has continued to build his business which remains successful.”
Advertisement
Advertisement

Prompt, multidisciplinary care helps navigate the complexities of a rare condition

New research adds to understanding of an understudied link

The Head & Neck Institute will make its initial footprint in the newly constructed BioRepository building
Collaboration critical to a successful resection

Randomized controlled trial finds no quality-of-life benefit after standard pituitary tumor surgery

Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor

Case study illustrates the potential of a dual-subspecialist approach

Evidence-based recommendations for balancing cancer control with quality of life