Patient with cerebral palsy undergoes life-saving tumor resection
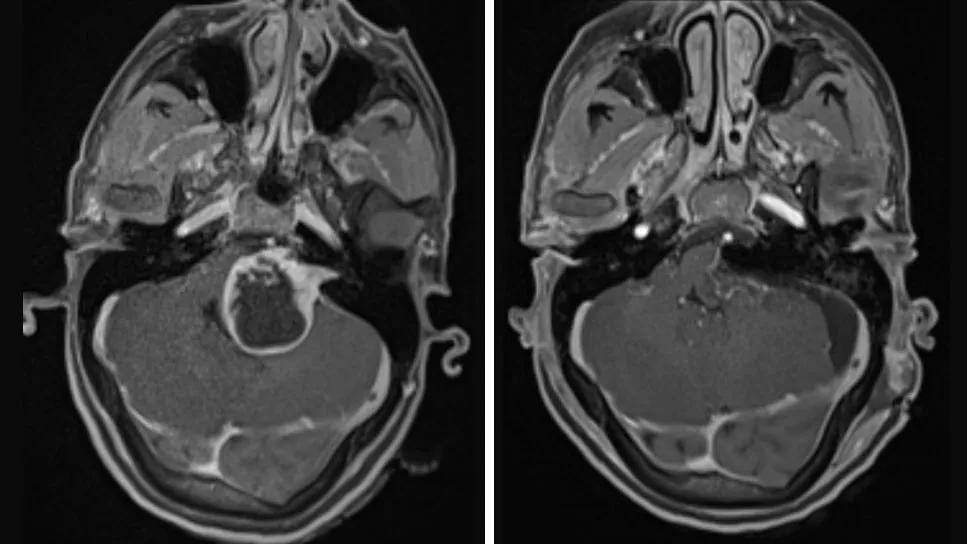
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d495f4a8-cf86-41c7-b54f-bd58f9aaaeda/vestibular-schwannoma-case-huynh)
Vestibular Schwannoma pre- and post-operative CT scans
A patient in her mid-20s with a history of cerebral palsy and GI issues presented to one of Cleveland Clinic’s regional emergency rooms. The patient was quadriplegic, deaf and nonverbal, but she had become increasingly lethargic and was experiencing increasingly severe abdominal issues including decreased appetite, nausea and vomiting. The attending emergency department physician ordered an extensive workup of diagnostic tests, including abdominal and cranial CT scans. On the CT scan, her radiologists discovered a large brain tumor and notified the neurosurgery team.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The patient was transferred to the ICU at Cleveland Clinic Main Campus the following day. The patient was not able to maintain her airway, a sign that cranial pressure was increasing, and was intubated to protect her airway. The patient’s intracranial pressure was found to be very high (greater than 30 cm of water), and an emergency external ventricular drain was performed to reduce the intracranial pressure.
The tumor was diagnosed as an acoustic neuroma, also known as a vestibular schwannoma. Once the emergency drain was placed, the neurosurgery team coordinated with the head and neck surgery team to plan the tumor resection. The team also decided to perform a permanent internal shunt, a type of procedure to divert the brain fluid that had been blocked, to help with long-term control of the patient’s cranial pressure.
A multidisciplinary team including neurosurgeon, Pablo Recinos, MD, and Mark Bassim, MD, the Section Head of Otology and Neurotology at Cleveland Clinic planned the surgery. Dr. Recinos would be responsible for removing the tumor, and Dr. Bassim would assist with the approach by opening the ear canal to remove the portion of the tumor in the internal ear canal. Another neurosurgeon, Sarel Voster, MD, was also involved in initially performing the creation of the internal fluid diversion.
A few days prior to the tumor resection, Dr. Voster performed an endoscopic third ventriculostomy surgery to reduce and stabilize the patient’s cranial pressure. The pressure continued to spike, so Dr. Recinos decided to move up the tumor resection surgery. However, Dr. Bassim was unavailable on the planned day, so another neurotologist, Anh Nguyen-Huynh, MD, was called to assist, despite already being in the middle of another vestibular schwannoma surgery with a different group of surgeons.
Advertisement
“For this particular case, my role was to open the internal ear canal so Dr. Recinos could access the tumor,” explains Dr. Nguyen-Huynh. “The tumor had filled up part of the internal ear canal and expanded into it, but the largest portion was deep to the ear canal in the brain compartment.”
Dr. Recinos began the surgery by opening the back of the head and removing the bulk of the tumor. Once Dr. Recinos had removed as much of the tumor as he could, Dr. Nguyen-Huynh stepped in to open the internal ear canal and removed the remainder of the tumor.
A postoperative MRI revealed complete gross resection of the tumor.
“There were a couple of aspects to this case that made it particularly challenging,” explains Dr. Nguyen-Huynh. “It’s not unusual for patients with a large tumor to experience weakness or difficulty walking early on, so they’ll often seek medical attention soon after which leads to earlier diagnoses. However, this patient has cerebral palsy and is quadriplegic. Vomiting is another symptom that typically raises a red flag, but her history of GI issues likely also concealed that there was something else going on.”
He continues, “In this case, the tumor was cystic, so she experienced extracranial pressure in a short amount of time. However, since the patient is nonverbal and deaf, it was only when her behavior changed, and she became lethargic that there was concern. It's very rare in this day of age to see a large tumor present all of a sudden like with her case.”
Dr. Nguyen-Huynh states that while this is one of the more complex cases he has encountered, the team-based approach used throughout this case reflects the typical standard of care at Cleveland Clinic. Having a team of surgeons with overlapping skill sets allowed him to step in when the original surgeon wasn’t available.
Advertisement
In Dr. Nguyen-Huynh’s first case, the team took a translabyrinthine approach, which meant he would be more involved from the beginning. On the other hand, Dr. Recinos used an extended retrosigmoid approach, performing most of the surgery initially, with Dr. Nguyen-Huynh joining near the end.
“The familiarity that our teams have with each other— neurosurgery and neurotology — means that we can be fluid in our roles and assignments,” he says. “On that particular day, I was asked to step in for my colleague, and even though I was already operating on another patient, we could coordinate everything logistically and still treat both patients very safely. Dr. Recinos didn’t need me while he initially worked on the large part of the tumor outside of the inner ear. So, we were able to coordinate everything so that I wouldn’t be needed until after I was done with my other case. Being in an environment where we support each other, collaborate effectively, and deliver comprehensive care to our patients is something that I don’t take for granted.”
Advertisement
Advertisement
Detailed surgical process uncovers extensive middle ear damage causing severe pain and pressure.
The rare condition can cause structural damage if untreated
Complex procedure highlights the power of coordinated care across spinal, thoracic and vascular surgery
Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor
Case study illustrates the potential of a dual-subspecialist approach
Evidence-based recommendations for balancing cancer control with quality of life
Study shows no negative impact for individuals with better contralateral ear performance
HNS device offers new solution for those struggling with CPAP