Recent FDA approval opens doors for new neurostimulation therapy

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/bab15ff3-b74a-475c-b81e-d92ef90a1693/16-NEU-782-Back-Pain-650x450_jpg)
back pain
Cleveland Clinic is among a limited number of healthcare systems using a new closed-loop spinal cord stimulation (SCS) device for patients experiencing intractable back and leg pain.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The U.S. Food and Drug Administration granted approval in March 2022 to Saluda Medical, a medical device manufacturer, for use of Evoke® Spinal Cord Stimulation System, a novel technology that adjusts in real time to optimize neuromodulation therapy.
Cleveland Clinic pain specialist Sherif Costandi, MD, has been a principal investigator for research on Evoke, which began in 2017. Cleveland Clinic patients currently have access to the treatment through enrolling in a study. A commercial launch in October 2022 will include 10 centers nationwide, including Cleveland Clinic.
Costandi’s clinical experience leads him to believe the technology represents a significant improvement in pain relief potential. Five years of trials at Cleveland Clinic have produced about 40 successful results, he says – some of them life-changing.
“I had a patient who had had many interventions for back pain, including injections and multiple surgeries,” Dr. Costandi says. “She had limited use of her back, and her quality of life was very limited. She came to me seeking a last-resort pain pump. Instead, with closed-loop stimulation, we were able to get between 98.5% and 100% relief during her trial.”
The patient regained her ability to walk her dog and to stand for sustained periods of time, says Dr. Costandi. “We’re working with her now to strengthen her muscles and her core so she can continue to improve,” he says. “It’s a big goal, yet we will be able to get there.”
Spinal cord stimulation has been in use since the 1960s, and improvements over the decades have included development of smaller and better implantable devices. Before Evoke, says Dr. Costandi, implanted SCS systems worked by sending fixed stimulation output to nerves in the spinal cord, modulating the perception of the pain. This open-loop system delivers information in one direction only.
Advertisement
Evoke, by contrast, is the first available device that can read, record the electrical activity of the spinal cord and then respond by real time self-adjustment of the electrical firing of the SCS.
“This new closed-loop system has the ability to measure the neural response within the SCS, which is variable from one person to another and varies within individuals as they move,” Costandi says. “Evoke measures electrical response and its variations, then adjusts its own output based on those variations.”
The system receives neural feedback 100 times per second. This has the advantage of providing optimal stimulation, Dr. Costandi says – neither over- nor under-stimulating the spinal cord.
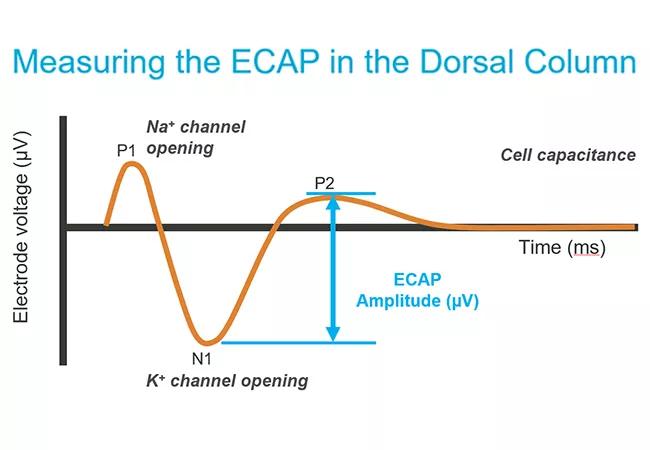
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0fe0a696-8013-463d-965b-3ed7a1f83d53/22-PAI-2851942-CQD-650x450-1_jpg)
In general, SCS therapy requires a two-stage procedure: trial and implantation.
During initial trial phase, guided leads are placed in the spinal column. Test stimulations are used to ascertain correct placement of the leads, and the device is programmed to identify the minimum amount of pressure that can be felt by the patient and the maximum that can be withstood. Those parameters define the therapeutic window. “Our goal is to keep the patient in this window for maximum benefit of the therapy,” says Dr. Costandi.
The patient goes home for a week to 10 days with an external battery-powered transmitter and engages in normal activities, including things they have not been able to do because of pain.
“When they come back, we talk about what were we able to accomplish and how much relief they have been getting,” says Dr. Costandi. “What’s different with this therapy is that we have a record of how much the patient used the therapy. Patients are able to stay within the therapeutic window almost 99% of the time.”
Advertisement
If the trial is successful, the patient is brought back for implantation. The leads are secured to the spine and a pocket is created in the flank for the battery. “Placement of the Evoke is done exactly the same as any with other stimulation devices,” Dr. Costandi says. “Their software is far superior. Their leads have the capability of measuring the electrical activity of the spinal cord, but it does not affect placement or require extra training.”
A study published in the March 1, 2022 issue of JAMA Neurology compared patients receiving traditional open-loop stimulation therapy to the closed-loop system and tracked performance over two years. Of the closed-loop group, 79.1% experienced 50% or greater reduction in overall pain. Of the open-loop group, 53.7% achieved 50% or greater reduction in pain. Quality of life improvements included physical and emotional functioning, sleep and reduction or elimination of opioids.
“One of the hypotheses about loss of durability with traditional SCS is that it may be caused by overstimulating the spinal cord, although that has not been proven yet,” says Dr. Costandi. “The hope is that this individualized therapy will make relief from SCS more durable.”
Advertisement
Advertisement
Guidance from the largest cohort of SEEG-confirmed insular epilepsy patients reported to date
Ethical guidance provides guardrails so medical advances benefit patients
OCEANIC-STROKE results represent long-sought advance in secondary stroke prevention
Two studies from Cleveland Clinic may help advance the technology toward broader clinical use
Distinct MRI signature includes lesions beyond the corpus callosum, features predictive of vision and hearing loss
An argument for clarifying the nomenclature
An expert talks through the benefits, limits and unresolved questions of an evolving technology
Recommendations on identifying and managing neurodevelopmental and related challenges