Today’s research helps illuminate tomorrow’s needs
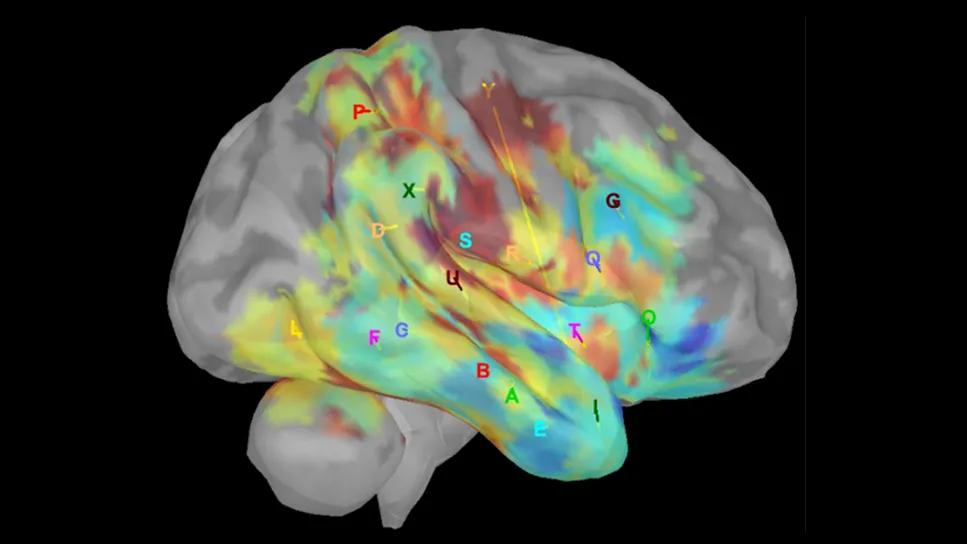
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1fb123d5-2710-49a9-b424-37286dfbf477/Neuro-building-advancing-neurorehab-hero)
Electrophysiological brain activity of a patient during an experimental sensory-motor neurorehabilitation task for epilepsy.
Above: Electrophysiological brain activity of a patient during an experimental sensory-motor neurorehabilitation task for epilepsy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The neuroprosthetic device some individuals wear today to overcome foot drop after a stroke didn’t even exist when Susan Linder, DPT, PhD, began her career.
“When I started practicing, we used a plastic brace in the shoe to keep the foot elevated and prevent dragging a toe or tripping,” says Dr. Linder, Director of Clinical Research for Physical Medicine and Rehabilitation at Cleveland Clinic. “The technology that has emerged since then stimulates the muscle, and it is programmed to know where the leg is in space and to lift the foot at the proper time.”
That one progression is emblematic of the impact technology has had on neurological care in recent decades — a period that also has seen the development of robotic exoskeletons, brain-computer interfaces, wearable sensors and deep-brain stimulation. These and other advancements, and the promise of more to come, are why Cleveland Clinic’s new 1 million-square-foot Neurological Institute building is designed with tomorrow in mind.
“We have a singular opportunity in the rehabilitation space,” says Paul Marasco, PhD, whose lab at Lerner Research Institute’s Department of Biomedical Engineering studies the sensory nervous system and movement feedback for bionic limbs. “Other domains of rehabilitation are relatively well-established, but neurorehabilitation is very much in the early growth phase. We will accelerate this.”
In this article, the latest in a series devoted to the new Neurological Institute building, Drs. Marasco and Linder speak to the ways that advancing neurorehabilitation has been baked into the planning. Previous installments cover distance health, the role of digitization in advancing clinical care and discovery, and the inpatient experience.
Advertisement
Cleveland Clinic’s Department of Physical Medicine and Rehabilitation incorporates all therapy disciplines and provides about 700,000 rehabilitation visits each year at the health system’s Main Campus, acute-care hospitals, inpatient rehabilitation hospitals, outpatient therapy sites, skilled nursing facilities and through the Center for Connected Care.
When the new Neurological Institute building opens at Main Campus in 2027, rehabilitation will occupy about a quarter of the ground floor. Clinicians, therapists and patients will work side-by-side with the researchers who are developing leading-edge solutions for individuals being treated for stroke, traumatic injuries, surgeries, multiple sclerosis, epilepsy, Parkinson’s disease and more.
Research has historically been more difficult to integrate with rehabilitation medicine than with other clinical departments, Dr. Linder explains. “Now we will be integrated geographically, so we will have more opportunities for organic collaboration. It will allow clinicians who don't do research to tap into some of our knowledge, technology, equipment and other resources, and vice versa. This is a two-way street.”
For example, she adds, a therapist working with a patient who has an unusual gait pattern might benefit from novel tools still in the research stages.
Research and clinical rehabilitation will have discrete work areas, but they will be separated by windows instead of walls, introducing literal transparency to what those on each side are working on so that opportunities for integration remain top of mind.
Advertisement
Because state-of-the-art technology is built into every aspect of the new building, those working on the neurorehabilitation space were challenged to think beyond the moment.
“Instead of placing a traditional therapy space into this new, high-technology building, we looked at what we’re working on in research that might be five or 10 years ahead of the clinical world,” says Dr. Linder. “Then we asked how we could help the clinical world catch up a little bit faster, and how we could design a space to ensure we're not outdated as soon as we open.”
Innovation will be immediately apparent to patients when they arrive and digitally check in for their appointments at an automated assessment center. Modules include a hallway outfitted with high-speed cameras to capture gait metrics as patients pass through on the way to their appointments. Data is immediately sent to the patient’s practitioner. “These cameras will measure not just their gait speed, but how much their knee, ankle, hip and trunk move – all sorts of parameters that can really inform their disease status. And we can intervene earlier,” Dr. Linder says.
Part of the planning team’s strategy was equipping the clinical rehab spaces with technologies of today while building infrastructure to support future technology. Virtual reality, for example, already figures prominently in key areas of movement disorders research and therapy.
“We're also talking about doing real-time integration of data streams that are coming from the individual, and then projecting those into the clinical workspace,” says Dr. Marasco. “We actually put a gait lab into the treatment space. So we allocated space for a clinically integrated research gait lab that then exists around all of the different real-time patient interactions faster.”
Advertisement
Suspension devices for supporting patients during gait training will replace rail-based systems that require therapists to hold the patient. Suspension systems allow for movement on any plane and in any direction, replicating real-world environments.
The future of neurorehabilitation research will continue to be driven by the quest to close the gap in understanding how the brain changes and how to administer therapy that truly changes the brain, Dr. Linder says.
“There are a lot of high-level technologies that are helping us start to understand how we control the brain, how the brain changes, that we did not even think of a decade ago," she says.
These are what Dr. Marasco calls some of the most difficult problems in neurological care.
“The thing that we do really well at Cleveland Clinic is take on all of the hardest problems — the stuff that's super challenging,” he says. “In the new building we will be able to facilitate the integration of tools that are more technically challenging into the clinical workflow. We will learn efficiencies, we will learn clinical needs, and we can help with implementation. We're able to bring things that are future-focused into the current reality.”
And while clinicians and researchers face different questions on a day-to-day basis, Dr. Marasco says that Cleveland Clinic’s patients-first culture sets the stage for collaborative relationships.
“Even though we all do different things, even though we all have different work that we do, everyone here shares the common goal of helping patients,” he says. “That just knocks barriers down automatically.”
Advertisement
Advertisement
Novel ‘assessment center’ will be a partner in care by serving as an engine of structured data collection
What it’s like working in neurology critical care and what to consider before entering the specialty
Case series links catastrophic outcomes to therapy initiation within 48 hours post-procedure
Scientific program chair reflects on what may resonate longest from this year’s neurosurgery conference
Tasked-based therapy improves social connection and quality of life
Neurology nursing calls for skill, emotional intensity and more
Input from these central stakeholders is leading us to design for healing and hope
Subtle information gleaned from clinical examinations prompted concern