Co-management increases opportunities for research and education

by Anthony Fernandez, MD, PhD, and M. Elaine Husni, MD, MPH, Codirectors of the Cleveland Clinic Dermatology and Rheumatology Collaborative Care Center
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
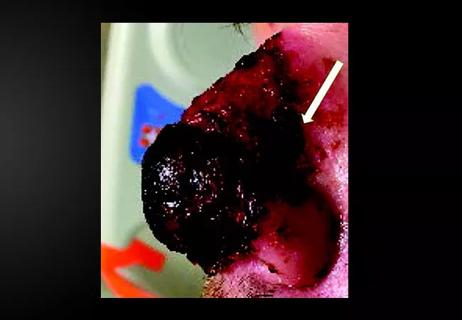
A 49 year-old woman with psoriasis and psoriatic arthritis (arthritis mutilans subtype) sought care at Cleveland Clinic for both active joint and skin symptoms. She was on infliximab at presentation, but was developing ongoing erosive disease.
Finding good treatment options for this patient was not straightforward. While living in China she contracted latent tuberculosis, which required adequate treatment before she could safely be started on many of the systemic medications that would be expected to improve her psoriatic disease. The patient sought the opinions of internists and dermatologists, who prescribed topical treatment. She also consulted with rheumatologists, who felt that although she continued to experience mutilans, there was no active joint disease activity to justify biologics in the setting of TB. The patient’s quality of life worsened and she withdrew from social activities due to flares of psoriasis and limited her travel due to worsening joint pains she would suffer from long plane rides. Her joint exam remained quiet, with no active synovitis or enthesitis, but she did have persistent, intermittent right shoulder pain.
After evaluating the patient and discussing her case together, we initiated the patient on a systemic treatment (apremilast), which we felt had the efficacy and safety profile she needed. Although there are other treatment options that may have more robust response in terms of skin and joint efficacy, it took a collaborative approach with a dermatologist and rheumatologist to weigh the risks and benefits of further immunosuppression versus initiating another therapy and monitoring response. The patient’s shoulder pain was evaluated by an MRI after she failed conservative management, which we could have easily attributed to PsA, but after further evaluation, she required rotator cuff repair. Three years later, the patient remains on apremilast and continues to enjoy relief from the painful skin lesions and disabling joint symptoms she had suffered from previously.
Advertisement
Patients with psoriatic disease commonly have both skin and joint symptoms with heterogeneous presentations. Optimal treatment should rely on shared decision-making between patients with chronic inflammatory diseases and a multidisciplinary team that includes a rheumatologist and dermatologist.1,2
At Cleveland Clinic, we have historically taken a collaborative, multidisciplinary approach to patients with complex disease processes, such as PsA. Our collaborative dermatology-rheumatology clinic has increased connectivity between the two disciplines, improved patient outcomes, and increased opportunities for education and research.
Patients with both skin and joint symptoms of psoriatic disease report a significantly impaired quality of life compared with the general population, including greater emotional burden, worse health status, as well as increased disability and work impairment.3 However, patients, rheumatologists and dermatologists seem to perceive disease symptom burden and quality of life very differently. To better understand this variability, a study was conducted to survey these differences among the patient, the rheumatologist and the dermatologist, and to identify themes that could be improve health outcomes.
The DISCONNECT study analyzed the perceived quality of life impact of many psoriatic disease manifestations in a survey of 200 patients and 300 physicians.4 Although there was agreement concerning perceived bother of some psoriatic manifestations among patients and physicians, there were important differences in the perceived bother of other psoriatic manifestations. For example, patients and physicians agreed that joint pain, soreness and tenderness are among the most bothersome manifestations of psoriatic disease, but patients rated painful, inflamed or broken skin as being more bothersome than either rheumatologists or dermatologists. Furthermore, differences in perceived symptom bother were seen between rheumatologists and dermatologists. Relative to joint pain, rheumatologists were more likely to perceive other joint symptoms as bothersome, while dermatologists were more likely to perceive other skin symptoms as bothersome.
Advertisement
This study suggests that treatment by both specialists should have as a composite goal the improvement of both skin and joint disease activity, especially the symptoms or impairments felt to be most severe and/or most bothersome to the individual patient. This further suggests the need for both rheumatologists and dermatologists to listen carefully when asking patients about symptoms to get a complete understanding of their needs, and supports that a multidisciplinary clinic enables a dermatologist and rheumatologist to directly communicate with each other and the patient in a setting that optimizes chances of implementing a treatment plan that aligns with the patient’s needs and goals.2
Being together and making decisions together about which medicines may best treat the entire patient – what’s going on from the skin, joints and other organ systems – can be very beneficial for patients. Real-time co-management and connectivity may enhance this assessment, accelerating the pace of putting the patient on appropriate medication, switching or adding medications if we need to, patient education, etc., depending on the severity of the skin and joint issues.
Although we understand the pathophysiology of these immune diseases much more now than we did just 10 years ago, we still have an enormous need to better delineate their molecular pathways and be more precise in our treatment algorithms. With two physicians from different backgrounds and specialties in the same space, research concepts will emerge, offering more opportunities to grow cross-disciplinary research, and ultimately contribute to better understanding and treatment of these diseases.
Advertisement
Advertisement
Advertisement

Family history may eclipse sun exposure in some cases

Consider secondary syphilis in the differential of annular lesions

Persistent rectal pain leads to diffuse pustules

Two cases — both tremendously different in their level of complexity — illustrate the core principles of nasal reconstruction
Stress and immunosuppression can trigger reactivation of latent virus

Low-dose, monitored prescription therapy demonstrates success

Antioxidants, barrier-enhancing agents can improve thinning hair