Series of high-risk patients supports hybrid approach in well-chosen candidates
Hybrid treatment of tandem carotid artery lesions with carotid endarterectomy and ipsilateral carotid artery stenting can be safely performed in appropriately selected patients if careful attention is paid to distal carotid clamping before stenting. So finds a retrospective review of Cleveland Clinic’s experience with the approach, which revealed no perioperative deaths and a low risk of myocardial infarction (MI) and neurological events. The study was published in the Journal of Vascular Surgery (2019 Sep 10 [Epub ahead of print]).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“We use a hybrid carotid procedure that combines the best of both worlds of open and endovascular procedures,” says Sean Lyden, MD, Chair of Vascular Surgery at Cleveland Clinic. “Our experience demonstrates a low rate of adverse events despite a high-risk cohort.”
Tandem lesions of the internal carotid artery and proximal arch branch vessels are uncommon. This leaves uncertainty about the safest treatment approach, with mixed results reported in the literature. While open reconstruction of arch branch vessels is invasive, endovascular reconstruction is not always feasible.
Cleveland Clinic vascular surgeons use a hybrid approach that employs concomitant open carotid endarterectomy and proximal ipsilateral carotid artery stenting (see representative images below). Their recent study assesses the Cleveland Clinic experience with the procedure in 22 patients from its adoption in December 2007 through April 2017.
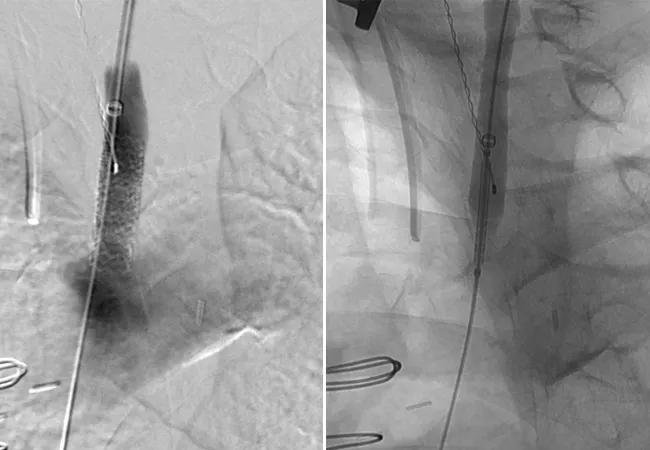
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/2cfeb2d8-85de-4083-8419-7abc661c1bce/20-HRT-106-Smolock-CQD-Hero_jpg)
X-rays showing retrograde proximal common carotid artery stenting with a balloon-expandable stent via carotid bifurcation endarterectomy patch access.
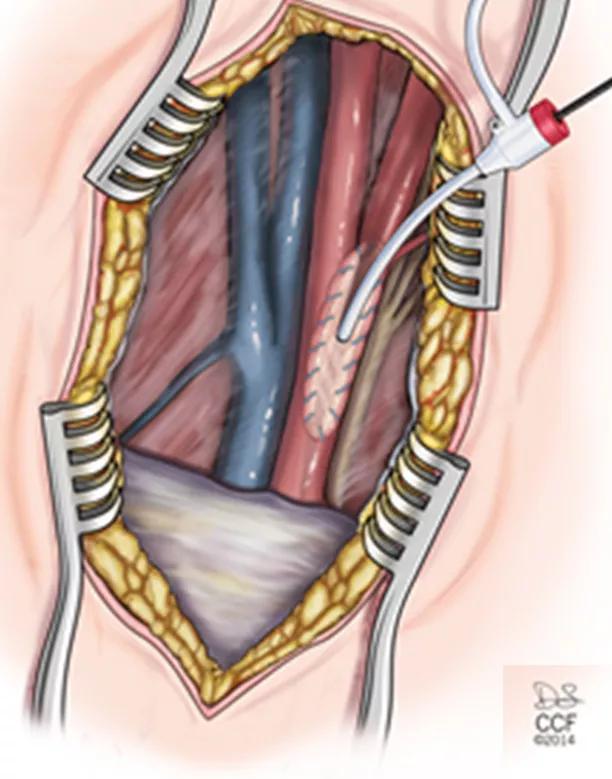
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4f1c6f35-06cd-4f0b-b154-355961e970ee/20-HRT-106-Smolock-CQD-Inset-3_jpg)
Illustration showing carotid patch retrograde sheath access in the context of the hybrid procedure.
The 22 patients were predominantly men (68%) and had a mean age of 70.0 + 6.1 years. They had a high rate of multiple comorbidities, with the most common being hypertension (86%), chronic obstructive pulmonary disease (56%) and diabetes mellitus (31%). In addition, 15 patients (68%) had a prior neurologic event and 12 (55%) were currently symptomatic.
Advertisement
All patients were either current (36%) or former smokers.
Many of the cases posed additional technical challenges. Nine patients (41%) had prior carotid endarterectomy or carotid artery stenting, with three having undergone prior neck radiation and three having had reoperative carotid surgeries.
Short-term outcomes. Technical success was 100%. Mean length of hospital stay was 2.6 + 2.0 days. Adverse events were as follows:
The death occurred in a 74-year-old man with end-stage renal disease on dialysis who had diabetes, chronic obstructive pulmonary disease and a prior MI.
Long-term outcomes. Average follow-up of the cohort was 2.8 years. Seven patients (32%) developed more than 50% restenosis, two of whom (9%) underwent reintervention due to symptoms. Survival was 89.5% at one year and 83.1% at three years. For deceased patients whose cause of death was known, death was secondary to conditions other than stroke.
The authors note that because this hybrid procedure is rarely performed, evidence of its safety and efficacy is limited to small series in which single events have a significant impact on outcomes data. Still, this single-center review indicates that the procedure can be performed successfully and safely by following the principles outlined below.
Select candidates carefully. In general, the procedure should be undertaken only in symptomatic patients. Otherwise, a more conservative approach with aggressive medical management is recommended. The patient in this series who had a perioperative contralateral stroke had a contralateral common carotid artery occlusion, which meta-analyses of carotid endarterectomy have shown to be a recognized risk factor for stroke and death. In many cases, however, risk is higher without treatment. Patients with end-stage renal disease are at particularly high perioperative risk of stroke and death relative to life expectancy, and most should be managed medically, especially if they have asymptomatic common and/or internal carotid artery disease.
Advertisement
Keep distal embolic protection foremost in mind.The following steps are recommended perioperatively:
Intervene for restenosis only in symptomatic patients. Restenosis can be expected, as patients with tandem lesions have advanced disease and those with a history of smoking are more likely to have recurrence. As with original candidate selection, symptoms should be more of a consideration than degree of stenosis when deciding whether to intervene.
“This patient population — with multiple comorbidities and risk factors — is at high risk both from their disease and from intervention,” comments Dr. Lyden. “In contrast to other single-center institutional data, our data show that with careful patient selection and targeted techniques to lower the risk of distal embolization, tandem carotid lesions can be addressed with acceptable risk.”
Advertisement
Advertisement

Scenarios where experience-based management nuance can matter most

Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients