Additional analyses of the two trials presented at 2023 ESC Congress
Additional analyses of two major multicenter trials of newer cardiovascular medications — bempedoic acid (Nexletol®) and mavacamten (Camzyos®) — have strengthened evidence of the agents’ clinical benefits.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The new analyses were presented in late-breaking science sessions at the 2023 European Society of Cardiology Congress in Amsterdam. Both of the studies analyzed were led by Cleveland Clinic investigators and coordinated by the Cleveland Clinic Coordinating Center for Clinical Research (C5Research).
One presentation focused on total cardiovascular events in the recent CLEAR Outcomes study of bempedoic acid in statin-intolerant patients, finding that the risk reduction conferred by the drug increased with each additional event among patients who experienced multiple cardiovascular events.
The other presentation shared longer-term results from the VALOR-HCM study of mavacamten in patients with highly symptomatic hypertrophic cardiomyopathy (HCM), extending follow-up to 56 weeks from the previously reported 32 weeks. Results showed that the drug continued to reduce patients’ need for septal reduction therapy and yielded sustained improvements in symptoms and left ventricular outflow tract (LVOT) gradients. These results were simultaneously published in JAMA Cardiology.
“Our C5Research academic research organization continues to provide the ability to take a deep dive into clinical trials to provide scientific insights that extend beyond the primary publication. These two presentations are illustrative of this approach to clinical trial analysis,” says Steven Nissen, MD, Chief Academic Officer of Cleveland Clinic’s Heart, Vascular & Thoracic Institute and a co-investigator in both the CLEAR Outcomes and VALOR-HCM studies.
Advertisement
The new report from the CLEAR Outcomes trial was a prespecified analysis of total cardiovascular events.
As detailed in the primary study report earlier this year (N Engl J Med. 2023;388:1353-1364), CLEAR Outcomes randomized a mixed population of 13,970 primary and secondary prevention patients with statin intolerance to oral bempedoic acid (180 mg/day) or matching placebo. The primary endpoint was a composite of cardiovascular death, nonfatal myocardial infarction (MI), nonfatal stroke or coronary revascularization. Over median follow-up of 40.6 months, this endpoint occurred in significantly fewer patients in the bempedoic acid group than in the placebo group (11.7% vs. 13.3%; hazard ratio [HR] = 0.87 [95% CI, 0.79-0.96]; P = 0.004), a 13% relative risk reduction.
Across the study cohort, 1,134 patients had one primary endpoint event and 612 patients had more than one event over the course of the study. The new prespecified analysis examined bempedoic acid’s effect relative to placebo on total events, including among patients with increasing numbers of events.
Among patients with more than one cardiovascular event, events beyond the first event broke down as follows:
When outcomes were analyzed according to first events versus total events, bempedoic acid demonstrated a statistically significant protective effect relative to placebo for the primary composite endpoint for both first and total events. This protective effect remained significant for all components of the primary endpoint except nonfatal stroke, where it trended toward significance for both first events and total events.
Advertisement
The total incidence of the primary composite endpoint was reduced by 20% with bempedoic acid relative to placebo (P = 0.0001). Total incidences of secondary endpoints were also reduced significantly with bempedoic acid, as follows:
Notably, bempedoic acid’s protective effect increased with increasing numbers of cardiovascular events, as follows:
“Although this was a prespecified analysis, its results remain hypothesis-generating,” notes Dr. Nissen. “Nevertheless, they suggest that in high-risk patients with statin intolerance, the clinical benefits of lowering LDL cholesterol and high-sensitivity C-reactive protein with bempedoic acid extend to reduction of total cardiovascular events, including incrementally increasing protection against repeat events.”
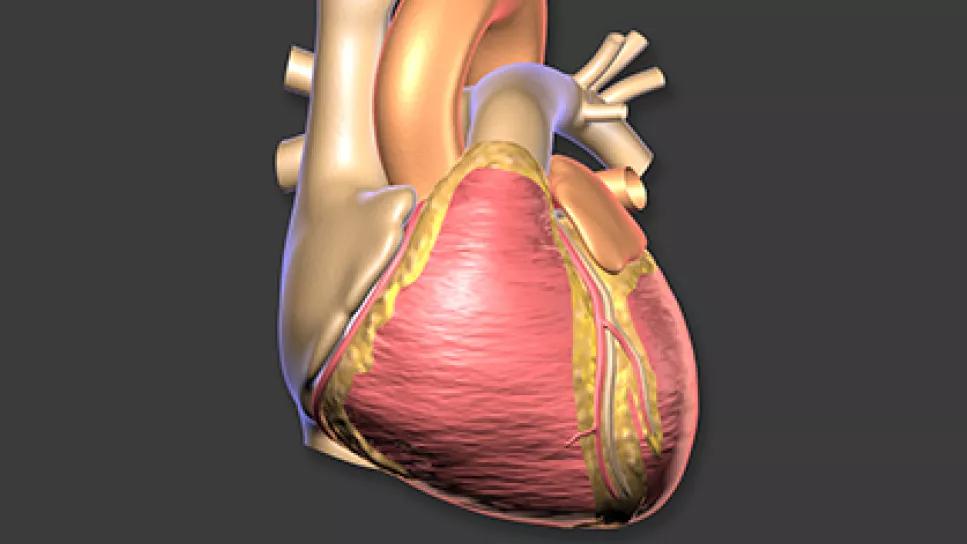
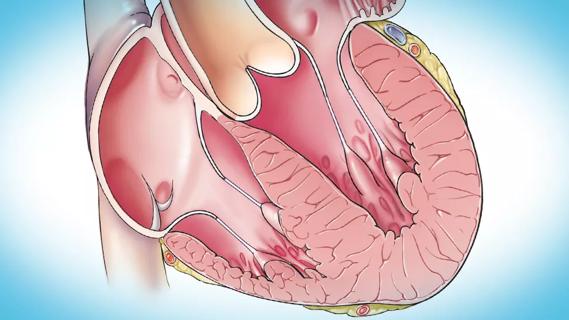
In April 2022, the cardiac myosin inhibitor mavacamten became the first medication approved by the FDA for treatment of symptomatic obstructive HCM. Approval was supported by 16-week results of the VALOR-HCM trial, a multicenter study that enrolled 112 patients with obstructive HCM and severe symptoms despite maximally tolerated medical therapy with disopyramide, a beta blocker and/or a calcium channel blocker.
Advertisement
Patients were randomized in a double-blind manner to oral mavacamten 5 mg/day or placebo; the mavacamten dosage was titrated up or down based on echocardiographic assessment of LVOT and left ventricular ejection fraction (LVEF). The primary endpoint was a composite of the patient’s decision to proceed with septal reduction therapy (SRT) or continued eligibility for SRT according to 2011 ACC/AHA guidelines.
Results at 16 weeks (J Am Coll Cardiol. 2022;80:95-108) showed a significant reduction in the share of patients meeting the primary endpoint (undergoing SRT or meeting SRT guideline criteria) with mavacamten relative to placebo. At that point, patients in the mavacamten group continued the drug and those in the placebo group were crossed over to mavacamten.
Results from the next interim analysis, at 32 weeks (Circulation. 2023;147:850-863), echoed and bolstered those from 16 weeks. An even smaller share of patients in the original mavacamten group met the primary endpoint of undergoing or meeting criteria for SRT (10.7%, vs. 17.9% at 16 weeks), and just 13.5% of patients in the placebo-to-mavacamten crossover group now met this primary endpoint, down from 76.8% at 16 weeks.
The new interim analysis reported results at 56 weeks as well as outcomes stratified by sex. Of the 112 enrolled patients, 108 qualified for assessment at 56 weeks. Results from 32 weeks were sustained through this time point, as follows:
Advertisement
Both groups also showed sustained improvements in resting and provoked LVOT gradients, NYHA class, biomarkers, left ventricular mass index, left atrial volume and quality-of-life scores at week 56.
Stratification by patient sex showed that mavacamten’s effects on eligibility for SRT, NYHA class improvement and LVOT gradients were comparable in men and women.
Notably, while 11% of patients experienced LVEF <50% during the study, after temporary therapy interruption, 75% of these patients were able to resume mavacamten at a lower dose with sustained LVEF recovery. “This underscores the need for careful echocardiographic monitoring during mavacamten therapy and the need for further long-term safety data,” says principal investigator Milind Desai, MD, MBA, Director of Cleveland Clinic’s Hypertrophic Cardiomyopathy Center and Vice Chair of Cleveland Clinic’s Heart, Vascular & Thoracic Institute.
He notes that echocardiograms were read at the study’s core lab for the first 32 weeks and on site thereafter. “We found significant correlation of LVEF and LVOT gradients between echocardiograms read on site and those read at the core lab, which suggests that echocardiographic monitoring will be a safe strategy in clinical practice,” he adds.
Overall, only four patients decided to proceed with SRT while on mavacamten therapy during the study’s first 56 weeks. “This suggests a strong patient preference for medical therapy over an invasive procedure,” Dr. Desai says, “although we must continue to monitor both safety and need for SRT over the longer term.” Follow-up in VALOR-HCM will continue through at least 128 weeks.
Advertisement

Emerging evidence suggests a patient-specific approach
Logistic feasibility supported for treating obstructive HCM under the REMS program

Multidisciplinary care for patients with immune-related adverse events

Cleveland Clinic will offer rapid, pinpoint airborne transport of medications and other medical items

Looking at the real-world impact and the future pipeline of targeted therapies

End-of-treatment VALOR-HCM analyses reassure on use in women, suggest disease-modifying potential

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Cardiac imaging substudy is the latest paper originating from the VANISH trial