Case study of a challenging diagnostic dilemma

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 54-year-old man who was on immunosuppressant therapy after a renal transplant two years prior presented with a recurrent ocular surface tumor of the left eye. About nine months prior, she had undergone excision of a red elevated nasal bulbar conjunctival mass. Recurrence of the lesion led to the referral.
Visual acuity of the involved eye was 20/50. We noted a yellowish-white multinodular episcleral mass involving the nasal quadrant and measuring about 10 x 8 x 6 mm with corneal involvement (including stroma) along the nasal limbus (Figure 1). Preauricular and submandibular nodes were not palpable.
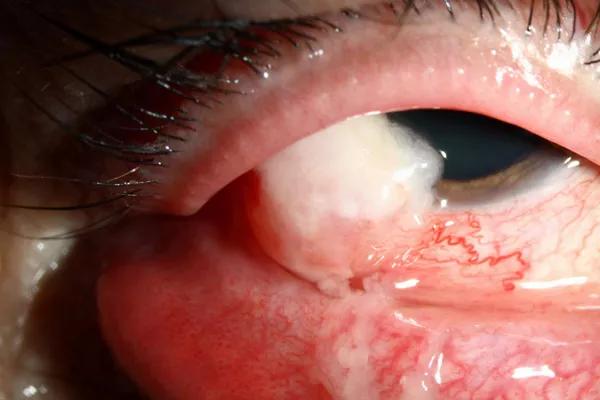
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/97911fc9-c4ce-46c3-b234-ca29fc00098b/17-EYE-1414-Singh-CQD-Inset-1_jpg)
Figure 1. Initial appearance at presentation at Cole Eye Institute.
We performed an excision of the conjunctiva, cornea and lamellar sclera, with cryotherapy to the conjunctival margins and closure using a free conjunctival autograft. Given the microscopic stromal invasion, episcleral brachytherapy to the tumor bed with 2 mm safety lateral margins was applied.
At six months, a superior marginal recurrence was noted at the 9-11 o’clock position that was treated with excisional biopsy of the conjunctiva and cornea via partial thickness sclera and corneal dissection, cryotherapy and episcleral brachytherapy. Six months later (12 months since first brachytherapy), an inferior marginal recurrence was noted at the 4-5 o’clock position. The patient was treated similarly to the prior two procedures.
One year after the last episcleral brachytherapy application, ectropion repair and symblepharon release followed by phacoemulsification for radiation cataract were performed. In total, three iodine-125 radiation episcleral plaques were used over a period of 49 weeks. A planned dose of 85 Gy at a depth of 3 mm was used for the first and second plaque, and 60 Gy at a depth of 4 mm was used for the third (Figure 2).
Advertisement
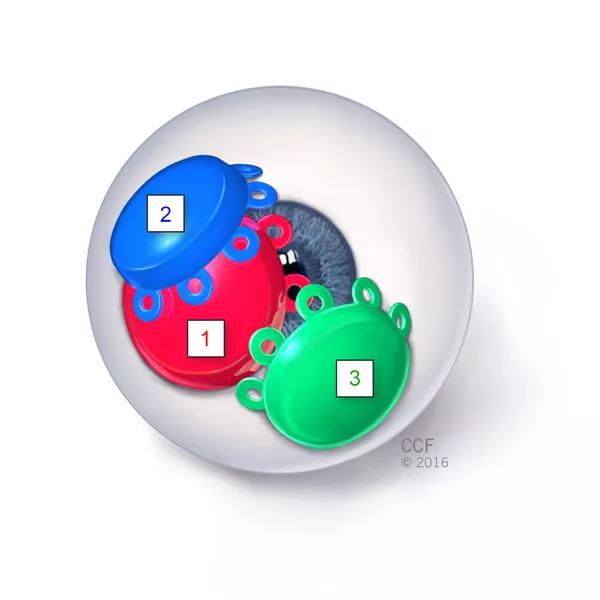
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ac4bed37-686a-4569-af5f-9da9cb418920/17-EYE-1414-Singh-CQD-Inset-2_jpg)
Figure 2. Schematic representation of position of three iodine-125 radiation episcleral plaques applied over a period of 49 weeks. A planned dose of 85 Gy at a depth of 3 mm was used for the first and second plaque, and 60 Gy at a depth of 4 mm was used for the third plaque.
Over the total follow-up of five years (four years since last brachytherapy application), the patient’s final visual acuity was 20/20 without evidence of local recurrence, radiation retinopathy or optic neuropathy (Figure 3).

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4e60eaa2-3fc6-4575-a138-24e4a6835a7e/17-EYE-1414-Singh-CQD-Inset-3_jpg)
Figure 3. Over the total follow-up of five years (four years since last brachytherapy application), the external appearance was satisfactory (A), visual acuity was 20/20 and there was no evidence of local recurrence (B) or radiation retinopathy (C).
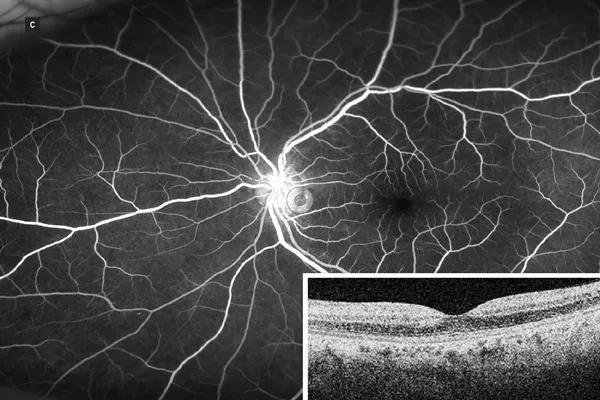
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a7bd358e-d7f4-478a-bbf3-85c197e5fb85/17-EYE-1414-Singh-CQD-Inset-4_jpg)
The histopathology demonstrated a neoplastic cell population with variably spindled to epithelioid cell morphology, predominantly with low-grade nuclei. There were areas of necrosis. Mitoses were 4-16 per 10 high-power fields. Immunoperoxidase stains showed strong and diffuse positivity for smooth muscle actin and negativity for H-caldesmon, desmin, myoglobin, S-100, melan A, HMB45, AE1/3 and CAM5.2 (Figure 4). In situ hybridization for Epstein-Barr virus was negative. The final diagnosis was consistent with myofibrosarcoma.
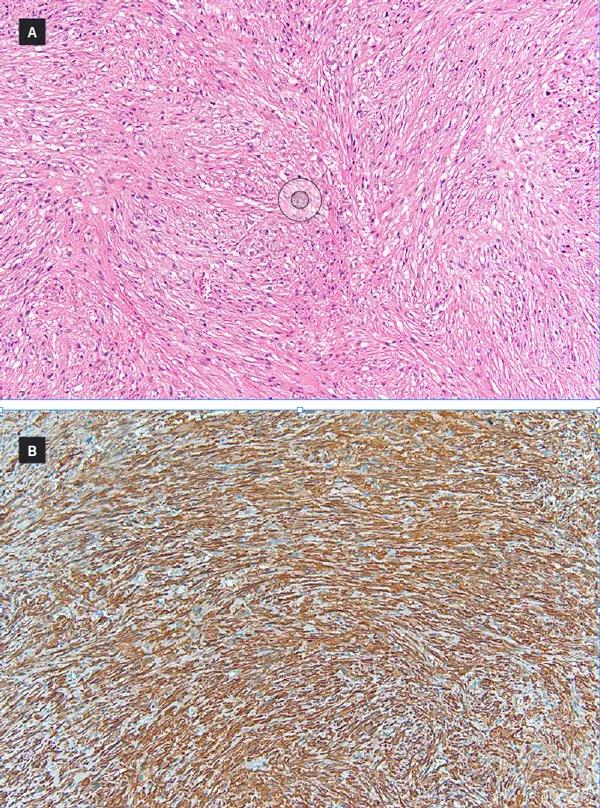
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e8c2e3da-b51b-4291-9a40-2c492b996ef0/17-EYE-1414-Singh-CQD-Inset-5_jpg)
Figure 4. (A) Histopathologic examination revealed cells with spindle nuclei in a fascicular pattern with poorly defined eosinophilic cytoplasm (hematoxylin and eosin, 100 X magnification). (B) Immunoreactivity to smooth muscle actin was positive (100 X magnification) and negative to H-caldesmon, desmin, myoglobin, S-100, melan A, HMB45, AE1/3 and CAM5.2 (not shown).
Advertisement
The diagnosis of myofibrosarcoma can be challenging because several lesions have similar histology. The differential diagnosis includes mesenchymal tumors such as leiomyosarcoma, spindle cell variant of squamous cell carcinoma (spindle cell carcinoma) and malignant melanoma. Our case was initially believed to be an invasive squamous carcinoma, pleomorphic sarcoma (malignant fibrous histiocytoma, myofibrosarcoma) and leiomyosarcoma, before a final diagnosis of myofibrosarcoma was established on the basis of histopathology along with a panel of immunohistochemical stains. To our knowledge, no prior cases of primary ocular or conjunctival myofibrosarcoma have been reported.
Figures reprinted and article extracted with permission. Platt SM, Schoenfield L, Basti S, Bryar PJ, Goldblum JR, Singh A, Singh AD. Recurrent conjunctival myofibrosarcoma managed with triple application of episcleral brachytherapy. Cornea. 2017 May;36(5):628-630. journals.lww.com/corneajrnl/toc/2017/05000.
Dr. Singh is Director of Ophthalmic Oncology at Cole Eye Institute.
Advertisement
Advertisement

Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma

Registry data highlight visual gains in patients with legal blindness

Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence

A look at emerging technology shaping retina surgery

A primer on MIGS methods and devices

7 keys to success for comprehensive ophthalmologists

Study is first to show reduction in autoimmune disease with the common diabetes and obesity drugs

Treatment options range from tetracycline injections to fat repositioning and cheek lift