New guidelines update recommendations
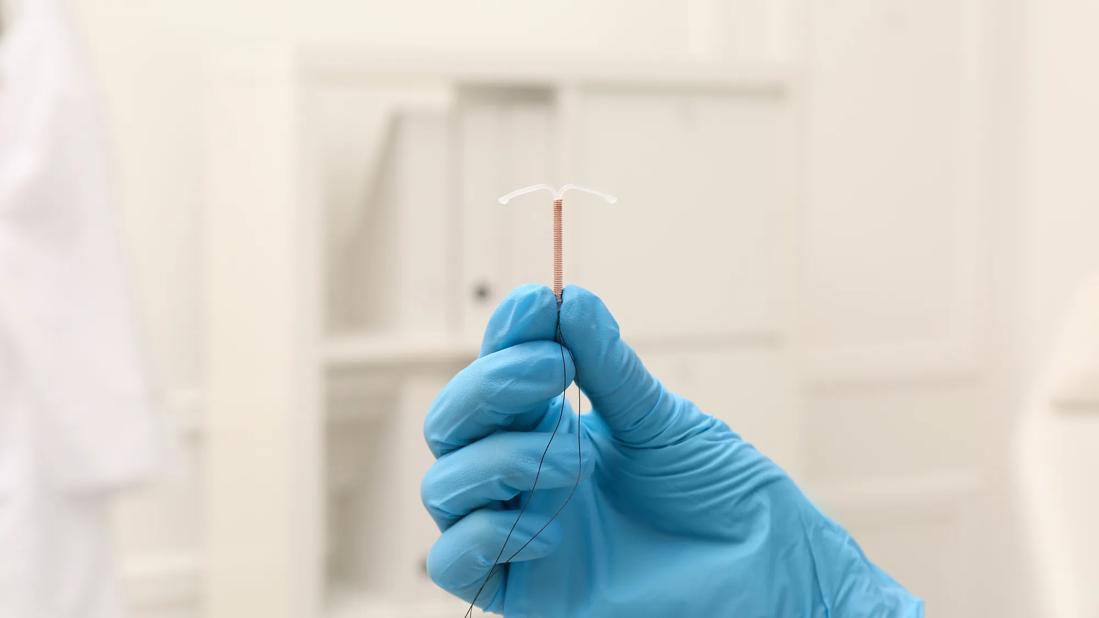
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/bf86cbd6-18ac-4a69-975a-a98c677d35bc/copper-intrauterine-device-1407069065)
copper IUD device being held by a gloved hand
Cancer survivorship rates and cancer diagnoses are both on the rise, and women are being diagnosed with cancer earlier in life. More than ever, there is a need for evidence-based contraceptive counseling tailored to the specific medical profiles and wishes of patients with cancers of all kinds.
In 2012, the Society of Family Planning issued Cancer and Contraception guidelines for treating cancer patients and survivors of reproductive age. This year, the Society published updated guidelines in the journal Contraception. The first author is Pelin Batur, MD, a staff physician in Cleveland Clinic’s Department of Subspecialty Care for Women's Health and whose areas of expertise include complex contraception.
The guidelines, prepared jointly with the Society of Gynecologic Oncology, emphasize the importance of providing person-centered recommendations and shared decision-making. They are published in three parts:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Historically, patients with cancer or who have had other complex medical histories were oftentimes assumed not to be appropriate candidates for hormonal contraception because of concerns about arterial or venous clots or liver effects,” says Dr. Batur. “There also generally has been hesitance to prescribe hormonal contraceptives to anyone who seemed like they have any increased risk of cancer.”
Even today, these beliefs continue to inform some decision-making, although the data does not support blanket restrictions on hormonal contraceptives.
“As a group, individuals with cancer or a cancer history have higher rates of unintended pregnancies, and they may have heavy bleeding or other gynecologic symptoms,” she adds. “They've already gone through so much. They should not be given unnecessarily limited options for contraception, heavy bleeding, premenstrual symptoms or dysmenorrhea. They should be afforded all their options.”
Within the realms of sexual activity, fertility and contraceptive preferences, people with cancer have distinct needs. Hormonal contraception and hormone-based intrauterine devices (IUDs) can increase the risk of some cancer recurring and influence the effectiveness of some cancer treatments. Some cancer treatments may alter the effectiveness of contraception. These considerations require communication between clinicians and patients to be clear and thorough, and they underscore the importance of shared decision-making.
Much new evidence has been published between 2012 and when the Society of Family Planning’s committee began working on the updated guidelines.
Advertisement
“We focused on hormonal contraception, which is what worries people, not barrier methods or nonhormonal IUDs,” says Dr. Batur. “Our initial literature search yielded over 16,000 results. When we looked specifically at hormonal contraception, four authors reviewed 5,484 references in addition to package inserts and FDA prescribing information.”
In developing the guidelines, the committee relied on expertise from clinicians in gynecological oncology, complex family planning, gynecologists and women's health internists so as to offer insights from people with multiple perspectives and variety of expertise.
“The guidelines had intense peer review — multiple rounds not only from the journal, but from medical societies,” says Dr. Batur. “And while most of the guidelines are aligned with U.S. Centers for Disease Control and Prevention (CDC) medical eligibility criteria, in areas where our recommendations favor more permissive shared decision-making, we let them know and got feedback from them. Where we did disagree, we clearly spell out why we thought there should be room for more shared decision-making.”
(Dr. Batur also discusses this topic on the Cancer Advances podcast.)
Seven overall recommendations can be found in the introductory portion of the Guidelines:
Advertisement
Detailed recommendations can be found in the portion of the Guidelines that address gynecologic and breast cancers, but here are some key takeaways:
Breast Cancer Recommendations. For those with histories of hormone receptor-positive, nonhormonal contraceptives are the first-line option. In cases of hormone receptor-negative cancer, clinicians and patients should engage in shared decisioning-making for hormonal contraception. Patients with increased risk for familial or hereditary breast and ovarian cancer should be provided access to all available contraceptive methods.
Ovarian Cancer Recommendations. For those with a history of or active ovarian cancer, access to all available contraceptive methods should be provided. Shared decision-making should be used with patients who have hormonally sensitive ovarian malignancies such as adult granulosa cell tumors, low-grade serous and endometrioid adenocarcinomas. Patients at high risk for ovarian cancer should be offered hormonal contraceptives with the aim of ovarian suppression for the prevention of ovarian cancer. Patients receiving estrogen-blocking therapy should avoid estrogen-containing contraceptives.
Uterine Cancer Recommendations. Those with a history of endometrial cancer should be provided access to all available contraceptive methods. Patients who have active endometrial cancer should be provided with shared decision-making for use of an IUD. Patients with a history of or active gestational trophoblastic disease should receive access to all available contraceptive methods after uterine evacuation in the absence of persistent intrauterine disease. Shared decision-making for IUD use should be used with those who have persistently elevated hCG levels or evidence of intrauterine disease.
Cervical Cancer Recommendations. Patients with a history of cervical cancer or active cervical dysplasia should be provided with access to all available contraceptive methods. Those with active cervical malignancy should be counseled against IUD placement.
Advertisement
The new guidelines also offer recommendations on contraceptive use for patients who have or have a history of a wide range of other cancers. In many cases, providing access to all available forms of contraception is recommended, including with certain forms of skin, blood, gastrointestinal, liver, lung, central nervous system cancer and more.
Advertisement
Advertisement
Mode of delivery does not affect patient satisfaction
A case-based discussion of efficacy, eligibility and use
Genetic variants exist irrespective of family history or other contributing factors
Percutaneous stabilization can increase mobility without disrupting cancer treatment
Simple score uses clinical factors to identify patients who might benefit from earlier screening
Use of GLP-1s and improving cardiovascular health lowers risk of hematologic malignancies
Sexual disorders affect patients across all cancer types
Largest study of its kind identifies three treatment exposures that contribute to risk