Study finds that 11% of those originally deemed ineligible for LASIK are now candidates

Evaluating patients for corneal refractive surgery eligibility is challenging, particularly because it’s crucial to recognize the subtleties of ectatic disease in its early stages. Additionally, these screenings, most of which use Placido-based corneal topography or Scheimpflug corneal tomography, are still mostly subjective. Corneal epithelial thickness mapping may add valuable insight into this process, according to a new study in the American Journal of Ophthalmology.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Relatively few surgeons are currently using epithelial thickness maps,” says the study’s senior author J. Bradley Randleman, MD, of Cleveland Clinic Cole Eye Institute. “The pure practicality of how a practice would be changed if it had this device or not has never really been evaluated, so we wanted to take a look and see in a reasonably well-defined study how often our surgical decisions were changing.”
High-frequency digital ultrasound and optical coherence tomography are both capable of producing a comprehensive epithelial thickness map. Dr. Randleman and colleague William J. Dupps, MD, PhD, routinely use Scheimpflug corneal tomography and epithelial thickness mapping in their clinical practice when evaluating patients for refractive surgery. The results are combined with patient-related factors (such as age, refractive error and corneal thickness) to determine surgical eligibility.
In the recent study, Drs. Randleman and Dupps re-evaluated (in a masked fashion) 100 consecutive patients who had been screened for refractive surgery at the Cole Eye Institute from February 2020 to September 2020. This re-evaluation took place six or more months after the patients’ initial clinical evaluation and imaging with both Scheimpflug tomography and anterior segment optical coherence tomography (AS-OCT).
The researchers independently assessed de-identified patient records for corneal refractive surgery eligibility using all of the initial evaluation information except the epithelial thickness maps from the AS-OCT imaging. They ranked surgical procedures — LASIK, PRK and SMILE — from most favorable to least favorable in terms of biomechanical impact on the patient’s cornea. Next, they looked at the patients’ epithelial thickness maps from the AS-OCT and reconsidered their evaluations.
Advertisement
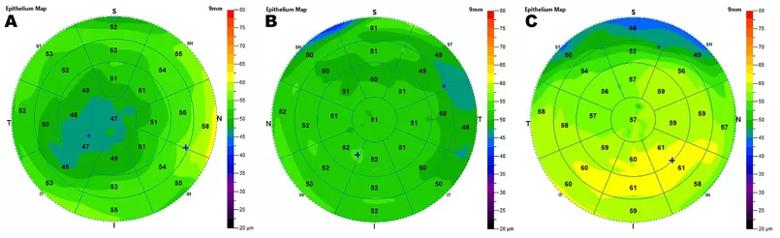
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d7805391-b5de-4ef8-ac2e-e7bbdef10e4b/22-EYE-2905316-CQD-_-Eligibility-for-refractive-surgery-Randleman_805x246_INSET_jpg)
Shown above: (A) Focally thin epithelium that would rule out laser vision correction; (B) Normal epithelial map; (C) Inferior epithelial hypertrophy that would rule in laser vision correction.
Overall, the researchers found that 82 of the 100 patients were candidates for corneal refractive surgery, with the remaining 18 patients determined ineligible. Eligibility for surgery changed in 16% of the patients after their epithelial thickness maps were considered — 10% initially deemed ineligible were screened in and 6% initially deemed eligible were screened out.
Additionally, the most favorable surgery for 16% of patients changed after their epithelial thickness maps were considered, and the ranking of the surgical procedures changed for 25% of patients. Eleven percent originally deemed poor candidates for LASIK were determined eligible, and 8% lost their eligibility for LASIK.
“We were surprised by the number of times the corneal thickness maps changed our surgical decisions,” says Dr. Randleman. “We thought the maps would add another level of confidence to our decision-making, but they were more impactful than we expected.”
It’s important to note that the researchers used corneal epithelial thickness mapping to screen in two-thirds more patients than they ruled out, adds Dr. Randleman.
“Screening patients in is equally as important as screening patients out,” he says. “If you’re very conservative, you may be choosing not to operate on a good number of people who would benefit from surgery and from no longer wearing corrective lenses. Using epithelial mapping to screen more patients in is potentially beneficial to your practice as well as your patients.”
Advertisement
Advertisement

Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma

Registry data highlight visual gains in patients with legal blindness

Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence

A look at emerging technology shaping retina surgery

A primer on MIGS methods and devices

7 keys to success for comprehensive ophthalmologists

Study is first to show reduction in autoimmune disease with the common diabetes and obesity drugs

Treatment options range from tetracycline injections to fat repositioning and cheek lift