EDEN analysis investigates electrophysiological changes after continuous dentate nucleus stimulation
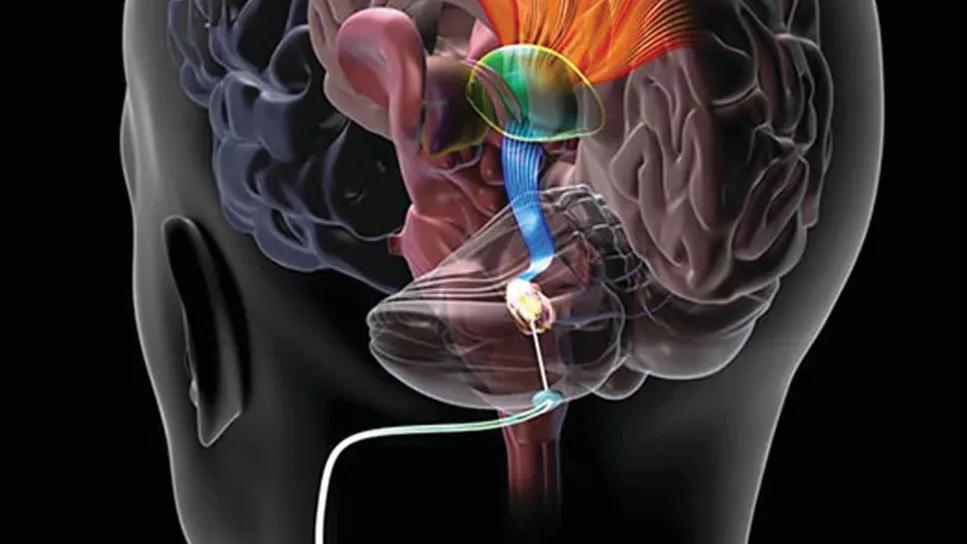
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/484b1e0c-6ddb-4c01-8549-324edb1ac742/deep-brain-stimulation-of-dentate-nucleus)
deep brain stimulation of dentate nucleus
Continuous deep brain stimulation of the dentate nucleus (DBS-DN) for four to eight months in stroke patients undergoing physical rehabilitation results in significant improvement in upper extremity function, and the improvement is accompanied by reduced cerebellar dependence for motor control. This finding, from a study of electrophysiological data from participants in the phase I EDEN trial, indicates that electrical stimulation deep in the cerebellum promotes cortical recovery in the area of the stroke lesion. The study was recently published in the Journal of Neuroscience.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The EDEN study design provided a unique opportunity to further investigate the underlying changes in the dentatothalamocortical pathway — an important network linking the cerebellum to the motor cortex — as a result of DBS-DN plus physical therapy,” says Raghavan Gopalakrishnan, PhD, MBA, of Cleveland Clinic’s Center for Neurological Restoration and a study author who led the electrophysiological investigations. “Our goal was to better understand how clinical improvement occurred in terms of brain function that could lead to objective biomarkers.”
“This project has given us exceptional insights into the function of a cerebello-cortical network after stroke and how DBS-DN modulates it,” adds the study’s senior and corresponding author, Andre Machado, MD, PhD, Chair of the Neurological Institute at Cleveland Clinic. “As participants improved, our results indicate that areas around the lesion in the cortex gained more function and depended less on the cerebellum for ordinary activities.”
The Electrical Stimulation of the Dentate Nucleus for Upper Extremity Hemiparesis Due to Ischemic Stroke (EDEN) trial (NCT02835443) — a single-arm, open-label study conducted at Cleveland Clinic — was a first-in-human study of DBS-DN for post-stroke rehabilitation. Its cohort consisted of 12 patients with a unilateral middle cerebral artery stroke that occurred one to three years prior to DBS-DN intervention and had resulted in moderate to severe upper extremity hemiparesis.
After implantation of the DBS lead, patients underwent four to eight months of continuous DBS-DN coupled with rehabilitation therapy, after which the lead was explanted. All patients who had at least minimal preservation of distal upper extremity motor function at baseline exceeded the threshold of clinical improvement after treatment, based on the Fugl-Meyer Assessment of upper extremity function and the Arm Motor Ability Test. Gains did not correlate with the time since stroke, and no serious perioperative or DBS-related adverse events occurred.
Advertisement
Trial results were published in Nature Medicine (2023;29[9]:2366-2374) and summarized in a ConsultQD post. EDEN set the stage for an ongoing multisite phase II trial, the RESTORE study (NCT05701280), which is expected to recruit 40 participants.
The current study on electrophysiological correlates of motor improvements after DBS-DN therapy was based on data from the EDEN study. Motor testing using a visuomotor block-tracking task was conducted at two distinct times: (1) after implantation of electrodes but before DBS therapy commenced and (2) after DBS therapy was completed but before explantation.
The study design allowed investigators to do the following simultaneously:
“In this way, we could observe the effects of combined DBS and physical rehabilitation at both the perilesional cortex and the cerebellar DN, which are tightly interconnected by the dentatothalamocortical pathway,” Dr. Gopalakrishnan explains.
Dr. Gopalakrishnan notes that in healthy individuals, the cerebellum is less active in the performance of routine tasks, such as lifting a cup of coffee to drink. However, if the cup starts to slip from one’s fingers, the cerebellum is activated for quick adjustment to avoid dropping it. In contrast, the cerebellum in stroke survivors is much more heavily involved in performing routine tasks, likely as a response to the motor impairment resulting from damage to the cortex.
Advertisement
Analysis of signals before and after DBS-DN and physical rehabilitation therapy revealed that the cerebellum became less involved in routine tasks and that activity increased in the perilesional cortex. So-called cortico-cerebellar coherence — i.e., neural communication between the DN and the perilesional cortex — was very high during routine repetitive motor tasks in patients at the time of implant and was much less pronounced at the conclusion of DBS therapy.
“The neurons destroyed by the stroke cannot be revived following therapy,” Dr. Gopalakrishnan says. “However, the perilesional cortex becomes more excitable following DN-DBS to pick up the majority of lost function, allowing the cerebellum to become less involved, which is what we might see if healthy individuals were to perform our task.”
He adds that the functional excitability of the DN and its connectivity with the ipsilesional cortex, especially in the low beta frequency, seem to be a predictor of motor outcomes following DBS-DN. This information is critical since it will allow the team to develop frequency-specific DBS.
“The electrophysiological findings from the EDEN study have given us an interesting window into mechanisms of motor improvement after DBS, and they support our therapeutic approach,” Dr. Machado concludes. “The EDEN trial has given hope to patients that significant gains are possible even years after a stroke, and it has taught us a little bit about how the brain responds to this novel treatment.”
This research was funded by the National Institutes of Health BRAIN initiative.
Advertisement
Advertisement
Promising preclinical research indicates functional motor recovery is durable
First-in-human trial demonstrates safety, encouraging functional response in chronic phases of recovery
Guidance from the largest cohort of SEEG-confirmed insular epilepsy patients reported to date
OCEANIC-STROKE results represent long-sought advance in secondary stroke prevention
Aim is for use with clinician oversight to make screening safer and more efficient
Tasked-based therapy improves social connection and quality of life
Despite less overall volume loss than in MS and NMOSD, volumetric changes correlate with functional decline
LAA closure may be compelling option in atrial fibrillation ablation patients at high risk of both stroke and bleeding