A new NAIMS consensus statement summarizes evidence, guides MRI investigation
Traditionally considered a disease of white matter, multiple sclerosis (MS) is increasingly recognized as also having important manifestations in gray matter that are detectable on MRI. The North American Imaging in Multiple Sclerosis Cooperative (NAIMS) recently issued a consensus statement (published online in Brain) reviewing the current knowledge and clinical relevance of deep gray matter injury in MS from an imaging perspective.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
To discuss this emerging area of interest, Consult QD caught up with neurologist Daniel Ontaneda, MD, PhD, of Cleveland Clinic’s Mellen Center for Multiple Sclerosis Treatment and Research, who served as lead and corresponding author of the NAIMS statement.
A: Since MS is a demyelinating disease, the focus of imaging in MS has naturally been on white matter. For several years, and partially based on more sophisticated MRI technology, evidence has been mounting that changes attributable to MS also occur in gray matter — both in cortical and deep regions — especially from early stages of the disease. We are now realizing that MRI findings of deep gray matter tell us something a little different about how MS injures the brain, and they provide more insight into disability.
A: Conventional MRI is useful to measure deep gray matter lesions and volume. Much data on deep gray matter lesions was initially described using 7T MRI, but thalamic lesions can also be seen at more conventional field strengths. Functional MRI, diffusion tensor MRI, relaxometry and MR spectroscopy can provide additional quantitative information from deep gray matter structures, and these measures correlate with disability. Machine learning techniques based on large data sets are expected to play an increasingly important role for analysis of deep gray matter structures and to improve identification of regions of interest.
A: MS focal lesions can occur in all deep gray matter nuclei, but they are most common in the thalamus, where lesions can be located along the surface of the ventricle (subependymal) or around blood vessels, where they have a more ovoid configuration (perivascular). Lesions show demyelination as well as varying degrees of inflammatory changes; they tend to have less of an inflammatory pattern than white matter lesions but more so than cortical lesions. Similar to MS lesions in white matter, deep gray matter lesions can be classified according to the presence of inflammatory activity.
Advertisement
Volume loss is another important finding: deep gray matter atrophy occurs early in MS and precedes measurable whole brain volume loss. Volume loss is believed to reflect overall inflammatory activity and is associated with disability and cognitive outcomes. Volume measurements currently are mostly useful for research, and we recommend that MRI endpoints be incorporated into clinical trials. Their utility for clinical practice still faces some obstacles. For instance, not enough is known about variability, owing to technical differences in image acquisition, and clinical standards need to be determined that account for age, treatment status and measurement error.
A: The thalamus is the deep gray matter region that has been studied most in MS. Thalamic lesions can be found by microscopy and high-field MRI in more than two-thirds of MS cases. Pathologically, focal thalamic lesions exhibit neuronal loss, demyelination and axonal transection. The following demyelinating lesion types have been characterized (Figure 1):
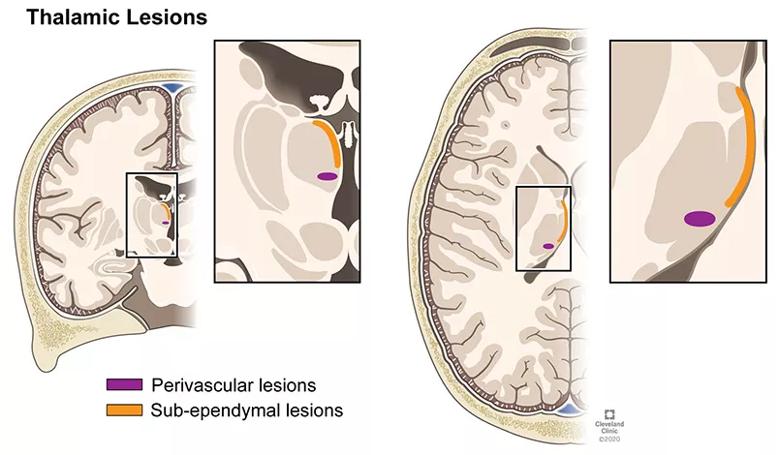
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d6f0c07d-9676-479e-acbd-eb9f7513e676/21-NEU-2210809_thalamic-lesions-in-MS_805x470_jpg)
Figure 1. Demonstration of thalamic demyelinating lesion types. Reprinted from Ontaneda et al., Brain. https://doi.org/10.1093/brain/awab132. © 2021 The Cleveland Clinic Foundation.
Thalamic volume loss in particular is also an important early indicator of MS. It can occur in adults, in children and in clinically isolated and radiologically isolated syndromes, even while whole brain and total gray matter volumes may still be preserved.
Advertisement
With the close interconnectivity of white and gray matter, injury to one affects the other. Multiple mechanisms of thalamic neuronal loss are possible, with white matter injuries potentially leading to volume loss of the deep gray matter (Figure 2).
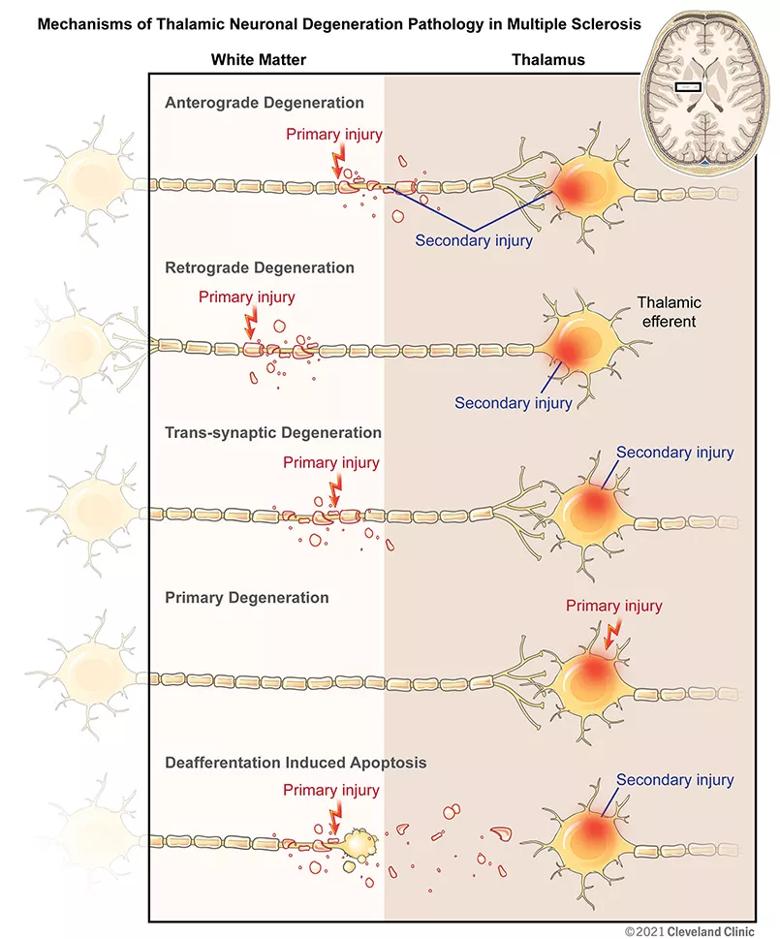
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/890e29a5-05e8-4943-b356-c9f31ec7883e/21-NEU-2210809_thalamic-neuronal-degeneration-MS_805x969_jpg)
Figure 2. Mechanisms of thalamic neuronal degeneration pathology in multiple sclerosis. Reprinted from Ontaneda et al., Brain. https://doi.org/10.1093/brain/awab132. © 2021 The Cleveland Clinic Foundation.
A: Yes — a number of disease-modifying therapies have been found in placebo-controlled clinical trials to reduce thalamic volume loss. Disease-modifying therapies targeting gray matter may one day prove useful, particularly in younger patients early in the disease and for addressing specific clinical implications — for example, cognitive changes. Preferential effects of treatments on deep gray matter can add important insight into mechanisms of injury and will be an important area of research.
Advertisement
Advertisement
A case study in pairing imaging acumen with subspecialty expertise to yield answers and symptom relief
Guidance from the largest cohort of SEEG-confirmed insular epilepsy patients reported to date
Ethical guidance provides guardrails so medical advances benefit patients
OCEANIC-STROKE results represent long-sought advance in secondary stroke prevention
Two studies from Cleveland Clinic may help advance the technology toward broader clinical use
Distinct MRI signature includes lesions beyond the corpus callosum, features predictive of vision and hearing loss
An argument for clarifying the nomenclature
An expert talks through the benefits, limits and unresolved questions of an evolving technology