Study highlights exceptional survival rates and improved quality of life
When you think of locally advanced cancer of the hypopharynx, do you automatically think of surgery for treatment? For decades, this was standard practice. However, new research is giving patients a viable alternative to surgery with promising results.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
While hypopharyngeal tumors aren’t common in the U.S., the problems associated with their growth and treatment are. For decades, physicians have been faced with the challenge of providing effective treatment while maintaining a reasonable quality of life.
Due to the precarious location of hypopharyngeal tumors, they tend to cause swallowing problems. When they cause blockages in the throat, food and beverages end up spilling over into the larynx. Eventually, patients have difficulty swallowing their own saliva, which could lead to aspiration, aspiration pneumonia, weight loss, etc.
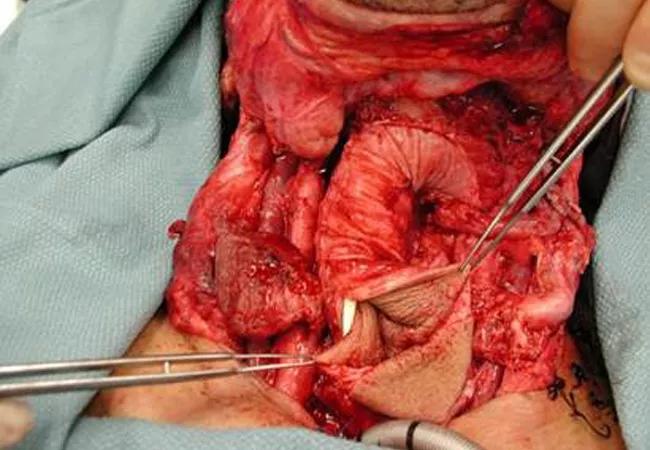
Through the 1980s, surgery was the primary treatment for locally advanced cancer of the hypopharynx. Surgeons would remove the larynx and pharynx (including the hypopharynx). Then, they would reconstruct the throat to restore the patient’s ability to swallow (as shown in image above).
While surgery was effective at controlling the disease, issues involving recurrence, survival and quality of life abounded. For example, many patients recurred with distant metastases and had 5- and 10-year survival rates around 50 percent. The reconstruction techniques were challenging and often created long-term functional issues. For example, some patients would get food stuck in the reconstructed pharynx and could not tolerate an oral diet, which led to the addition of a G-tube for long-term management. All patients required a lifelong tracheostomy after surgery.
With the advent of chemoradiation protocols for head and neck cancer, Cleveland Clinic physicians offered chemoradiation as a secondary treatment option when surgery was refused by patients with cancer of the hypopharynx. These patients often experienced positive outcomes, allowing researchers to generate some preliminary, defined data.
Advertisement
Building off the success of a laryngeal preservation trial as well as their own data, Cleveland Clinic researchers conducted an observational, retrospective study of patients with locally advanced squamous cell carcinoma of the hypopharynx. According to Brian Burkey, MD, MEd, Professor and Vice Chairman of Cleveland Clinic’s Head & Neck Institute, this was the longest published median follow-up in this population.
The study involved a group of 54 patients who were treated with definitive chemoradiation at Cleveland Clinic over a period of 27 years. The patients had stage 3 or stage 4 locally advanced squamous cell carcinoma of the hypopharynx.
The study yielded the following results related to survival and toxicity:
Following nonsurgical treatment for hypopharyngeal tumors, the majority of patients tend to recur locally in the throat or neck. “To achieve nearly 80 percent 10-year local control with chemoradiation is quite spectacular and very consistent with results seen with laryngeal cancer,” explains Dr. Burkey.
In addition, the study revealed promising functional data related to speech and swallowing. “While some patients needed a G-tube during treatment, only about 15 percent needed the G-tube for long-term use after treatment,” notes Dr. Burkey. “Basically, our patients had an 80 percent chance of preserving their voice box and an 85 percent chance that their voice box complex would be functional.”
Advertisement
“Our excellent tumor control combined with exceptional functional results are very favorable when compared to the literature and help validate organ-preservation strategies for patients with hypopharyngeal tumors,” says Dr. Burkey. “These results give our patients additional options for treatment that maximize quality of life and remind physicians to consider nonsurgical options during tumor boards.”
According to Dr. Burkey, two factors likely impacted the successful outcomes for patients involved in the study. First, over 90 percent of the patients received the right amount (at least two doses) and the appropriate type of chemotherapy with radiation therapy. Second, about half of the patients had relatively small (T1 and T2) primary tumors.
Additional research is needed to compare surgery and chemoradiation when treating hypopharyngeal tumors. Future studies could involve multiple institutions and even lead to the development of alternative organ-preservation therapies for head and neck cancer, perhaps utilizing immunotherapy.
Advertisement
Advertisement

Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor

Case study illustrates the potential of a dual-subspecialist approach

Evidence-based recommendations for balancing cancer control with quality of life

Study shows no negative impact for individuals with better contralateral ear performance

HNS device offers new solution for those struggling with CPAP

Patient with cerebral palsy undergoes life-saving tumor resection

Specialists are increasingly relying on otolaryngologists for evaluation and treatment of the complex condition

Detailed surgical process uncovers extensive middle ear damage causing severe pain and pressure.