A study of the procedure’s efficacy is cause for reflection, not rejection
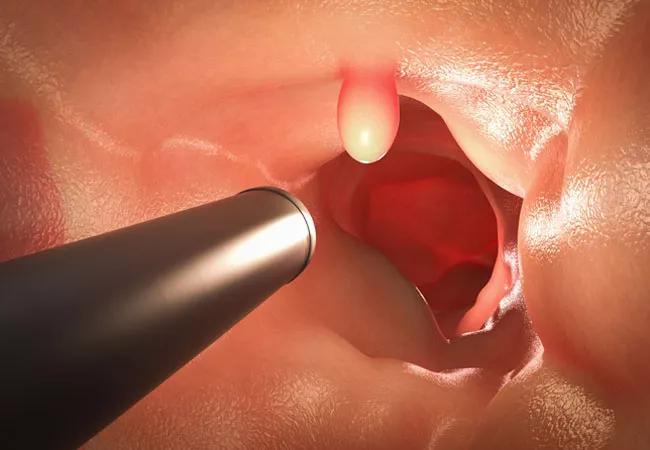
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/86e31aaa-259d-46be-a4e6-9c5303bf14af/22-DDI-3348194-CQD-NEJM-Colonoscopy-Effectiveness-Study-hero_jpg)
22-DDI-3348194 CQD-NEJM Colonoscopy Effectiveness Study hero
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
New research assessing colonoscopy’s benefits in population screening is drawing lots of attention and debate.
The general consensus, both from the European study’s authors and in much of the initial media coverage, is gloomy. The trial’s overall results show colonoscopy produced only a modest reduction in colorectal cancer risk and did not significantly decrease cancer mortality. More than 450 study participants had to be invited to undergo screening in order to prevent a single case of colorectal cancer within the study’s 10-year follow-up period.
Based on those findings, the procedure long touted as the gold standard for colorectal cancer prevention and early detection is “not the magic bullet we thought it was,” the study’s lead researcher, University of Oslo gastroenterologist Michael Bretthauer, is quoted as saying. “I think we may have oversold colonoscopy.”
“Surprising and disappointing,” declares an editorial in the New England Journal of Medicine, which published the research.
“Screening Procedure Fails to Prevent Colon Cancer Deaths in Large Study,” proclaims the headline on the Bloomberg news service report, echoing the tone of much of the early coverage.
While the study’s intent is admirable, I think its results are being mischaracterized, and some important context and caveats are being overlooked. The findings are more a reflection of ongoing public hesitancy about the procedure, not its efficacy.
In my view, colonoscopy remains our best tool to stop colorectal cancer. We should continue to encourage our patients to take advantage of the procedure while helping them understand its risks and limitations. We also should be prepared to address the questions and skepticism about colonoscopy that this study, known as the Nordic-European Initiative on Colorectal Cancer (NordICC) trial, is likely to create.
Advertisement
To do that, some background is helpful.
The current evidence that justifies colonoscopy’s predominant role in colorectal cancer screening in the U.S. comes from observational cohort studies of colonoscopy recipients. Collectively, the results estimate that the procedure decreases cancer incidence by 40%-69% and reduces cancer mortality by 29%-88%.
Those estimates may be too high, however, in part because cohort studies are subject to confounding and selection bias. They don’t, for example, account for the less-than-perfect adherence to screening that happens in the real world, or the likelihood that those who undergo preventive screening are healthier than the general population.
The NordICC researchers sought to design a randomized, controlled trial that would mimic a population screening program, resulting in a more realistic estimate of colonoscopy’s effectiveness.
The researchers chose an approach called an intention-to-screen analysis, in which subjects in a population registry were randomly assigned either to receive an invitation to undergo a free screening colonoscopy or to receive usual care, meaning an invitation to virtual screening but no offer of colonoscopy.
The benefit of the intention-to-screen design is that it avoids confounding and selection bias, because participation is randomized and the people who receive invitations to undergo screening can consent or decline to undergo colonoscopy, just like in real life.
The drawback, as the study authors acknowledge, is a potential underestimation of colonoscopy’s effectiveness, since the cohort being analyzed includes not only those who elect to be screened but those who choose not to undergo the procedure. Colonoscopy can’t be effective if it’s not utilized. If participation is less than 100%, counting nonparticipants when analyzing colonoscopy’s effectiveness skews the results downward.
Advertisement
And that’s what happened. Before the trial’s start, the researchers expected that half the study cohort invited to undergo colonoscopy would comply, and that the procedure ultimately would reduce colorectal cancer mortality by 25% in the 10-year median follow-up period. In fact, only 42% of the invitees underwent screening. The resulting analysis of the combined cohort of 84,585 participants and nonparticipants found that colonoscopy reduced the risk of colorectal cancer by only 18% during a decade of follow-up, and that its impact on cancer mortality in the group was insignificant.
But when the analysis was adjusted to estimate colonoscopy’s efficacy if all screening invitees actually underwent the procedure, the results were considerably better: a 31% decrease in colorectal cancer risk and a 50% reduction in colorectal cancer-related deaths. The adjusted mortality risk reduction falls within the range of colonoscopy’s efficacy from observational cohort studies. The 31% decrease in cancer risk is somewhat less — though not dramatically so — than what the observational trials have found.
Comparing colonoscopy’s ability to reduce colorectal cancer risk in the intention-to-treat and adjusted per-protocol analyses to sigmoidoscopy’s efficacy in similar trials, the authors suggest that colonoscopy screening might not have a distinct edge over the less invasive and less expensive procedure. But sigmoidoscopy, of course, accesses only the distal colon, leaving a sizeable portion of the large bowel unexamined. And if sigmoidoscopy identifies cancerous or precancerous lesions in the distal colon, a follow-up colonoscopy is mandatory to look for proximal lesions.
Advertisement
Two other points about the study should be noted as we interpret the results.
First, colonoscopy’s effectiveness as a preventative and detection tool depends largely on the colonoscopist’s skill and experience. Individual gastroenterologists vary in their ability to identify precancerous polyps. The adenoma detection rate (ADR) — the proportion of screening colonoscopies a physician performs in patients age 50 and older that detect one or more histologically confirmed adenoma or adenocarcinoma — is the premier quality measure for colonoscopy.
The American Society for Gastrointestinal Endoscopy’s minimum benchmark rate for a U.S. physician’s ADR is 30% for male colonoscopy patients at average risk for colorectal cancer and 20% for female patients, with an overall average of 25%. Other professional societies recommend physicians’ ADRs be at least 25% for male patients and 15% for female patients.
But 29% of the colonoscopists performing screenings in the NordICC trial fell below the recommended minimum ADR level of 25%. Although the event rates were too small for detailed analysis, the study’s authors acknowledge that the variability in meeting the ADR quality threshold may have impacted the cancer detection rates they report. It is reasonable to think that, if all of the participating colonoscopists had met or exceeded the minimum ADR quality metric, additional precancerous lesions would have been detected, thereby improving the procedure’s cancer risk reduction rates.
A second consideration as we weigh the study’s findings – particularly those showing colonoscopy’s lack of significant impact on cancer-related deaths in the intention-to-treat analysis – is the trial’s 10-year interim reporting period.
Advertisement
Due to the typically slow progression of precancerous polyps, a decade probably isn’t a long enough span to fully capture colonoscopy’s risk-reduction benefits, especially regarding cancer mortality, which become apparent only on lengthier time scales. Two or three decades seems to be a more meaningful interval. It will be interesting to see whether colonoscopy’s impact numbers improve when the NordICC trial’s final analysis is completed at the 15-year end point.
Even before then, we can take steps to increase colonoscopy’s utilization. As clinicians, we can be more proactive in discussing colorectal cancer risk and screening measures with patients, helping them overcome reluctance and addressing misperceptions and concerns. Individualized reminders to undergo screening can be delivered more effectively via patient messaging in electronic health record systems and other means. Broader public health education campaigns to destigmatize the disease and emphasize prevention are vital and should be redoubled.
As someone who performs hundreds of colonoscopies each year, I am admittedly biased. But I continue to believe the procedure is our most effective way of preventing colorectal cancer, as well as diagnosing and treating the disease. Yes, it poses some risk and entails expense, time and medical resources. For those reasons, regular review and reassessment is important. In that sense, the NordICC trial is commendable
But it would be unfortunate if the takeaway was increased doubt about colonoscopy’s value. I will keep stressing its importance as the best available means of stopping a preventable disease.
Dr. Kanters is a colorectal surgeon in Cleveland Clinic’s Digestive Disease & Surgery Institute. She is board certified by the American Board of Colon and Rectal Surgery. Her research interests include identifying barriers to the delivery of high-quality care in colon and rectal surgery.
Advertisement
Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling
Simple score uses clinical factors to identify patients who might benefit from earlier screening
Radiation to the pelvis from cancer treatment made the traditional treatment path unavailable
Greater awareness among young patients is needed
Insights indicate that treatment may be beneficial beyond MSI-H tumors
New phase 1 trial showcases Neurological Institute’s interdisciplinary study capabilities
Cleveland Clinic Cancer Institute brings multidisciplinary care, precision oncology and clinical research to the United Arab Emirates
Surgery, chemotherapy improve outcomes among EOCRC patients