When artificial tears don’t bring relief
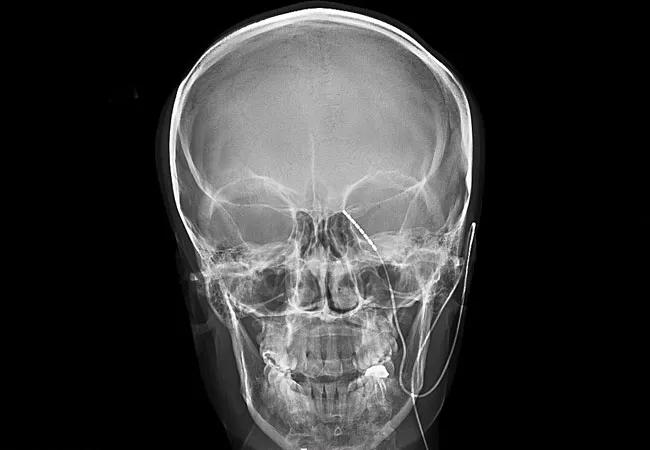
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5a7228e3-1285-49a4-be85-7f9bbe9add11/20-EYE-1958896-CQD-Cornea_jpg)
20-EYE-1958896-CQD-Cornea
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
One common ocular symptom associated with dry eye is pain. In a recent review of 144 patients with dry eye presenting to our clinic, 81% complained of some level of associated ocular pain, with 13% reporting severe pain (an intensity of at least 8 out of 10).
While pain is an important sensory and emotional experience that can serve as an alert to actual or potential tissue damage, “neuropathic pain” persists in the absence of the initiating insult. As such, persistent pain in the absence of signs of ocular surface damage, such as after adequate treatment of dry eye, can be considered a form of neuropathic pain.
Closer inspection of the subpopulation of dry eye patients who reported severe pain reveals important features that are relevant to the diagnosis of ocular neuropathic pain. Compared to dry eye patients with milder or no pain, those with severe pain tended to be younger and more likely to have had refractive surgery such as laser-assisted in situ keratomileusis (LASIK) or small incision lenticule extraction (SMILE).
Their medical history often included underlying depression and anxiety, as well as other chronic pain conditions such as fibromyalgia and migraine. In addition, a lower self-perceived overall health state was reported, with most patients rating their health as “bad.”
While the increased pain intensity was reflected in a higher Ocular Surface Disease Index (OSDI) score, corneal staining was less likely to be present in this population.
Finally, instillation of proparacaine eye drops resulted in improvement in pain in 50% of patients with severe ocular pain. This has been used as a test to differentiate peripheral from centralized neuropathic pain.
Advertisement
A common source of frustration to both physicians and patients is the lack of response to commonly used dry eye treatments. In fact, only 53% of patients with severe ocular pain reported any improvement in their symptoms with artificial tears, compared to about 90% in patients who reported mild or moderate pain. This response rate is even lower with various anti-inflammatory eye drops such as steroids, cyclosporine A and lifitegrast.
Among non-pharmacological treatments, sunglasses were found to be helpful by about two-thirds of patients with severe ocular pain, highlighting the commonly coexistent heightened sensitivity to light experienced by these patients. Hot compresses also were helpful, possibly exerting a direct neuromodulatory effect.
Interestingly, poor response to various oral agents including opioids, antidepressants, gabapentin and pregabalin was reported. Acetaminophen and nonsteroidal anti-inflammatories (NSAIDs) were most effective, with 60% of patients with severe pain reporting improvement with their use.
As such, it is important for ophthalmologists to optimize the ocular surface with the use of different eye drops and artificial tears, which will help in improving ocular pain in a significant number of patients. Hot compresses and sunglasses, particularly FL-41 tinted lenses, also are worth recommending. Analgesics, with the appropriate precautions, can be helpful as well.
But what about the remaining patients who do not respond satisfactorily to these treatments?
Advertisement
Pain signals from the cornea travel along the trigeminal nerve, which synapses with second-order neurons in the trigeminal subnucleus caudalis (Vc). These neurons project to the thalamus, where they synapse with third-order neurons that project to the sensorimotor cortex and paralimbal region, involved in the emotional aspect of pain. Targeting various sites along these pathways potentially can be beneficial in pain control.
Neuromodulation, using electrical stimulation or chemical agents to normalize nerve function, is one option. It has been used successfully as non-pharmacological therapy for chronic back pain as well as facial pain, among other conditions. Percutaneous placement of electrodes for the electrical stimulation of the trigeminal ganglion have resulted in complete resolution of symptoms in patients with severe ocular pain, but recurrence rates are high.
Alternatively, implantation of an intrathecal drug delivery system, providing microdoses of analgesics to the area of the trigeminal subnucleus caudalis at the C1-C2 level, resulted in adequate pain relief over a period of many years.
As we continue to seek effective treatments for the biological basis of chronic ocular pain, we must keep in mind the complex interplay of biological, psychological and social factors that perpetuate and even worsen the original symptoms. For optimal outcomes, Cole Eye Institute employs an interdisciplinary approach, simultaneously dealing with biological as well as psychosocial aspects of chronic ocular pain.
Advertisement
Dr. Sayegh is a staff member of Cleveland Clinic’s Cole Eye Institute. His specialty interests include cornea care with a focus on ocular surface disease.
Advertisement
Advertisement
A review of pathophysiology, risk factors, clinical presentation and treatment options
How computational tools and personalized biomechanics can improve keratoconus detection, ectasia risk assessment and surgical outcomes
Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma
Registry data highlight visual gains in patients with legal blindness
Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence
A look at emerging technology shaping retina surgery
A primer on MIGS methods and devices
7 keys to success for comprehensive ophthalmologists