Terrien’s marginal degeneration is underlying cause
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 55-year-old female from out of state presented to the Cleveland Clinic Cole Eye Institute for a chronic corneal perforation in her left eye. Three months prior, an outside ophthalmologist had performed pterygium removal. Surgery was complicated by corneal perforation, which was glued. Despite a second surgery to glue the perforation, the cornea still leaked, causing constant tearing and fluctuating vision, putting the patient at risk for infection. The patient sought a second opinion at the Cole Eye Institute.
At initial visit, there was a bandage contact lens in place over a large area of glue at the nasal limbus. The anterior chamber was shallow. After removing the contact lens, multiple leaks were noted at the edge of the glue. Careful examination of both eyes revealed subtle peripheral corneal thinning consistent with Terrien’s marginal degeneration, which was not previously documented and likely contributed to the perforation.
I removed the glue and found very thin underlying cornea with multiple perforations and no evidence of infection. I applied cyanoacrylate glue, which revealed new leaks outside the area of gluing. I glued over the new leaks, but the cornea remained Seidel positive. There were perforations noted in three clock-hours of peripheral cornea.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8e0eb84d-d8ed-4bf7-b384-2782bd92abb5/18-EYE-4344-See-CQD-Feat_jpg)
Figure 1: Intraoperative view prior to graft insertion. The glued patch is visible at 10:00. A second area of glue at 8:00 has already been removed. Peripheral neovascularization is consistent with Terrien’s marginal degeneration. A suture has been pre-placed and a Lewicky AC maintainer is in place.
Advertisement
It became clear that glue would not provide definitive repair. Traditional repair methods include eccentric corneal patch graft or penetrating keratoplasty. Her marginal degeneration meant her peripheral cornea was thin and could easily perforate during dissection or suturing. In addition, the perforated area was poorly defined and large (Figure 1). A traditional repair can easily become a bigger and longer surgery than anticipated in cases like this.
We discussed an unorthodox approach: an eccentric Descemet’s stripping endothelial keratoplasty (DSEK). The DSEK tissue would act as a patch over the multiple perforations. Advantages of this approach include sparing corneal stroma, avoiding sutures into thin cornea and speeding visual recovery.
DSEK has been described as a treatment for central perforations and corneal hydrops, but not multiple peripheral perforations, as in this situation.
I performed DSEK (without stripping) the following week. The graft was oversized to allow more extensive overlap in the periphery and avoid the graft edge splitting the pupil. I considered using a semicircular graft but worried about graft adherence with her brisk leak.
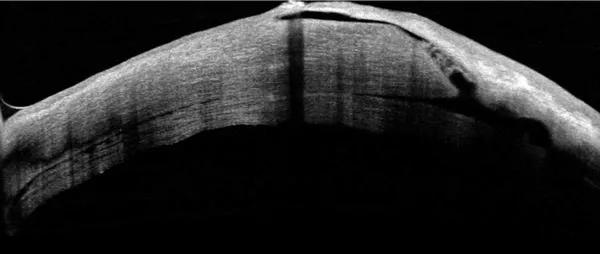
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/da86fd55-f95d-4156-a396-d49c185a166b/18-EYE-4344-See-CQD-Inset-1_jpg)
Figure 2: One week postoperative OCT shows partially attached DSEK graft. Note the extremely thin connection between healthy cornea and the thinned peripheral cornea. A fluid tract is allowing aqueous to create a bleb at the top of the image.
One week postoperatively, her chamber was shallow and her cornea Seidel positive. Optical coherence tomography (OCT) demonstrated a partially detached graft and an extremely thin host cornea (Figure 2). An in-office air bubble was successful in attaching the graft.
Advertisement
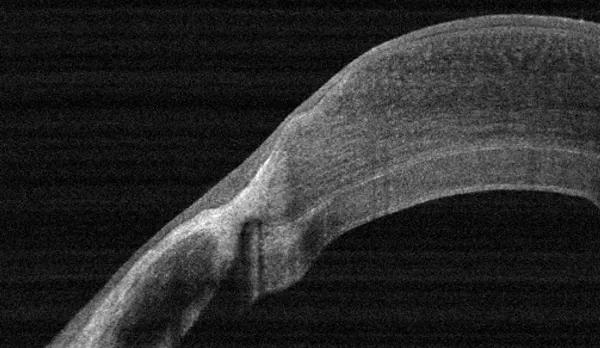
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/cf86e943-53d6-496a-adc6-7140519342ea/18-EYE-4344-See-CQD-Inset-2-1_jpg)
Figure 3: Three months after surgery, an intact cornea and clear DSEK graft can be seen.
Three months postoperatively, the patient’s cornea is watertight and chamber deep, and her vision corrects to 20/25. The graft remains clear (Figure 3). OCT demonstrates the DSEK graft plugging areas of perforation and thinning (Figure 4).
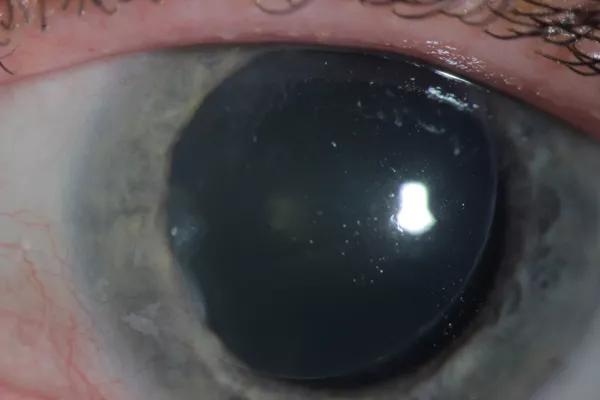
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6e7eed35-148a-4bca-9df1-6148eec66bc9/18-EYE-4344-See-CQD-Inset-3_jpg)
Figure 4: OCT image taken 3 months postoperatively shows attached DSEK graft which is plugging the extremely thin peripheral cornea.
Corneal perforations can be challenging to manage, particularly when the surrounding cornea is abnormal. In this case, careful examination of the other eye revealed not only the cause of her perforation but informed my decision to avoid traditional repair.
Thinking outside the box can improve patient outcomes and allows us to push the field forward.
Advertisement
Advertisement

Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma

Registry data highlight visual gains in patients with legal blindness

Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence

A look at emerging technology shaping retina surgery

A primer on MIGS methods and devices

7 keys to success for comprehensive ophthalmologists

Study is first to show reduction in autoimmune disease with the common diabetes and obesity drugs

Treatment options range from tetracycline injections to fat repositioning and cheek lift