Promising phase 2 study results
The thrombopoietin receptor agonist eltrombopag may accelerate platelet recovery in older patients being treated for acute myeloid leukemia (AML), according to the results of a phase 2 study presented at the 2019 American Society of Hematology Annual Meeting.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
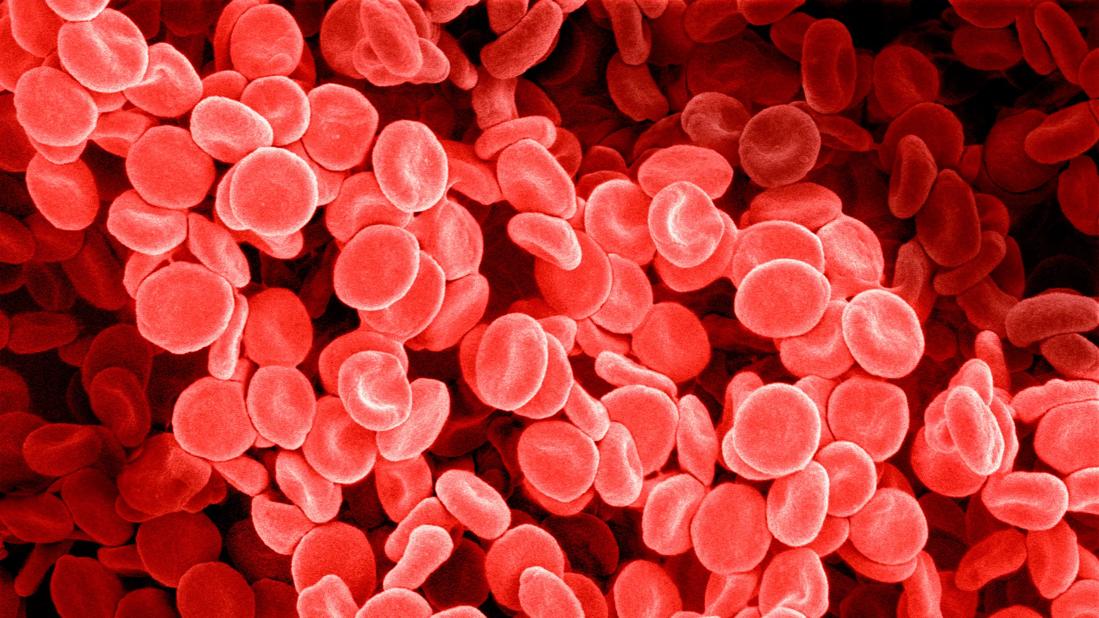
Consequences of delayed platelet recovery in AML patients undergoing intensive chemotherapy include increased risk of bleeding, increased need for platelet transfusion, alloimmunization to platelets and, importantly, delayed complete remission.
The single arm phase 2 trial enrolled 93 patients between September 2014 and September 2018; 31 patients ultimately met eligibility criteria. Patients, all over 60 years of age, received eltrombopag during 7+3 induction chemotherapy (IC) for AML in this trial if the day 14 bone marrow evaluation showed no evidence of leukemia. The proportion of patients who reached a platelet count of ≥ 50,000/µL by day 24 of IC served as the primary endpoint.
Researchers are cautiously optimistic about the potential of eltrombopag as they conduct additional analyses to evaluate durability of response and survival.
“Our interim analysis showed this to be safe and effective, and that continued to be the case in the final analysis,” says lead investigator Sudipto Mukherjee, MD, MPH, of Cleveland Clinic Cancer Center. “When we started this study six years ago, eltrombopag had never been tried before with 7+3 in up-front treatment of AML, so there was a lot we didn’t know.”
Eltrombopag has several characteristics that provided a rationale to test it in AML. It does not cause proliferation of leukemic blasts in in vivo experiments or xenotransplantation models, is not immunogenic and does not cause formation of platelet-neutralizing antibodies. Importantly, it stimulates production of platelets but does not cause activation of platelets.
Advertisement
“Delayed platelet recovery is a particularly severe problem in older people compared to younger patients with AML,” Dr. Mukherjee says. For that reason, the study’s eligibility criteria excluded anyone younger than 60 years of age, and the median age for the interim analysis was 67 years.
Enrolled patients had ECOG scores of 0 to 2, no active secondary malignancies and no evidence of marrow fibrosis at the time of diagnosis. Patients with acute promyelocytic leukemia, acute megakaryocytic leukemia and AML out of myeloproliferative neoplasms were also excluded. By CALGB criteria, 82% had intermediate cytogenetics, 9% had adverse karyotype and 9% had unsuccessful cytogenetic analysis. The majority of patients (84%) had de novo AML. IC treatment consisted of an anthracycline for three days followed by seven days of infusional cytarabine.
Thirty-one patients with a marrow blast count of < 5% on day 14 started daily eltrombopag treatment the following day. Participants received a dose of 200 mg per day. The study design allowed for dose escalation to 300 mg daily in case of slow platelet recovery.
Ninety-seven percent of patients met the primary endpoint with zero dose escalations. One patient reported a grade 3/4 toxicity, with the most common toxicities of any grade being maculopapular rash (28%), nausea (24%) and increased alkaline phosphatase (24%). No deaths occurred during treatment, and median overall survival time was 11.2 months (95% CI, 1.9, 14.8 months).
The median peak platelet count was 606,000/µL, and the median time to reach peak was 14 days. Median platelet transfusion requirement decreased from one unit every 3.6 days during IC to one unit every 4.8 days during eltrombopag treatment (P = 0.04).
Advertisement
“These results are promising for our older patients with AML,” says Dr. Mukherjee. “While we are continuing to monitor these patients for long-term outcomes, definitive answers to addition of eltrombopag in the upfront setting would require a confirmatory randomized clinical trial.”
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors