The search for new therapeutic targets
By Adam Brown, MD, Rula A. Hajj-Ali, MD, and Leonard H. Calabrese, DO
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Susac syndrome is an uncommon immune-mediated disease affecting the eyes, ears and brain in a triad of vision loss, hearing loss and encephalopathy. It’s unclear why these organs are targeted in this condition. In the eye, branch retinal artery occlusions (BRAO) cause ischemia to parts of the retina leading to patches of vision loss. In the ear, the most distal parts of the blood supply of the cochlea are affected. As a result, the patient experiences low frequency hearing loss, which can be more profound as the disease progresses. When the corpus callosum is involved the symptoms can be broad, ranging from headaches and mood changes to severe encephalopathy.
Diagnosis is often made following MRI of the brain; the ischemic lesions in the corpus callosum are referred to as “snowball lesions.”
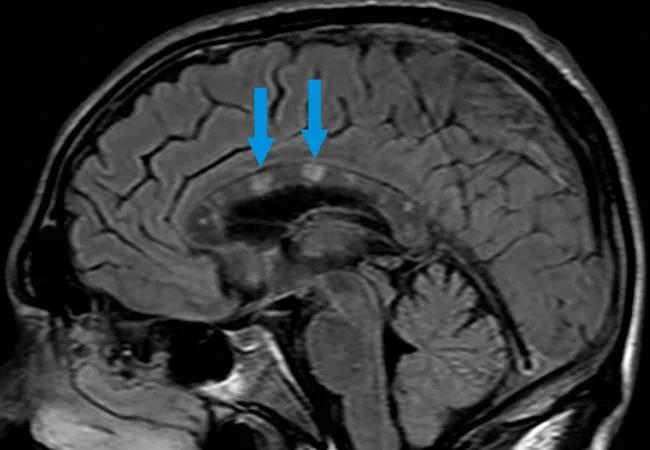
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/054559b5-e3e8-455b-83d8-9496b86ceaf2/20-RHE-1917015-Brown_SucacSyndrome-CQD-650x450-1_jpg)
Sagittal imagine of brain MRI demonstrating “snowball lesions” in the corpus callosum.
Susac syndrome is rare; the true incidence and prevalence are unknown. It is more commonly seen in females compared to males in a 3.5-1 ratio.1
Alterations of the blood vessels appear to be a focus of the disease pathology, causing decreased blood flow and ischemia to the affected organs. Usually when we’re talking about blood vessel pathology in rheumatology, we’re referring to a vasculitis, but in Susac syndrome the pathology is non-inflammatory, categorized as a vasculopathy and, more specifically, an endotheliopathy. An endotheliopathy occurs when the endothelial cells lining the blood vessel swell, occluding the lumen of the vessel as well as disrupting the normal cell-to-cell barrier of the vessel. The cause of the endothelial swelling is unknown. The histology of the small affected blood vessel of Susac syndrome demonstrates the endothelial swelling, but not an influx of immune cells that is typically seen in a vasculitis.
Advertisement
The approach to care for patients with Susac syndrome should be through a comprehensive team of specialists. At Cleveland Clinic, we have organized a team of specialists including ophthalmology, neuroimmunology, otolaryngology and rheumatology to care for these complex patients. Our Susac team at Cleveland Clinic has evaluated more than 100 patients for suspected Susac syndrome. Our team includes rheumatologists Adam J. Brown, MD, Leonard H. Calabrese, DO, and Rula Hajj-Ali, MD, neuroimmunologists Devon Conway, MD, and Ghulam Abbas Kharal, MD, MPH, ophthalmologists Sunil Srivastava, MD, and Sumit Sharma, MD, and otolaryngologists Erika Woodson, MD, Anh Nyguyn-Huynh, MD, and Thomas Haberkamp, MD. Considering the rarity of this syndrome, we will be working with multiple institutions to better understand this disease.
Currently, no robust outcome data exist to outline the disease course or what type of therapy is most effective in Susac syndrome. Treatment consists of aggressive immunosuppression, but the level of aggression depends on the severity of the disease. A patient with only a headache will not be treated as aggressively as a patient with vision loss and confusion.
One goal of our team is to better understand how patients with Susac syndrome do over time, as this will give us a better understanding of how aggressive treatment needs to be up front and how long therapy needs to be continued.
The pathophysiology of Susac syndrome is incompletely understood. A group in Germany has evaluated the role of CD8+ T cells in Susac syndrome, demonstrating the cells may have a role in the disease, expressing cytokines such as Tumor Necrosis Factor (TNF) and interferon.2 We have many medications that inhibit specific cytokines in rheumatology; if the cytokines involved in Susac syndrome are better elucidated, a more targeted approach to therapy could be pursued. One of the goals of our team is to better elucidate the underlying cytokine biology using cell-based techniques, such as transcriptomics, to gain insight into the roles of interferon and other cytokines in Susac syndrome, potentially providing new therapeutic targets for this rare condition.
Advertisement
Advertisement
Advertisement
Guidance from the largest cohort of SEEG-confirmed insular epilepsy patients reported to date
Ethical guidance provides guardrails so medical advances benefit patients
OCEANIC-STROKE results represent long-sought advance in secondary stroke prevention
Two studies from Cleveland Clinic may help advance the technology toward broader clinical use
Distinct MRI signature includes lesions beyond the corpus callosum, features predictive of vision and hearing loss
An argument for clarifying the nomenclature
An expert talks through the benefits, limits and unresolved questions of an evolving technology
Recommendations on identifying and managing neurodevelopmental and related challenges