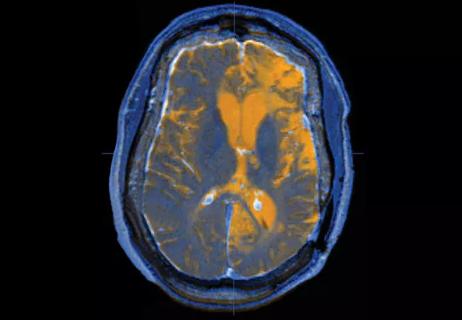
New guidance on penetrating head injuries, and noninvasive diagnostics get a nod in austere settings

As the number of U.S. neurosurgeons with subspecialty expertise in head injury is small, those few subspecialists carry an important charge of disseminating key advancements in their field to the broader neurosurgery community.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
One such subspecialist — Gregory Hawryluk, MD, PhD — takes that charge particularly seriously. In addition to his role as a neurosurgeon with the Level I Trauma Center at Cleveland Clinic Akron General Hospital, Dr. Hawryluk is Medical Director of the Brain Trauma Foundation (BTF) and leads the development of the BTF’s numerous head trauma guidelines.
When Consult QD recently checked in with Dr. Hawryluk about notable developments in his subspecialty, he identified two broad trends that loom largest in his mind: (1) new insights into penetrating head injury care and (2) emerging guidance on care in austere environments and the rise of noninvasive diagnostics.
Both trends involve developments stemming from so-called military-civilian translation, or the historical dependence of civilian neurotrauma practice on insights gained from neurosurgeons practicing in war theaters and combat zones. “There is a long-standing recognition that the military has unique experience with the most extreme forms of traumatic brain injury and other forms of neurotrauma that few civilian neurosurgeons see,” Dr. Hawryluk explains. “Our subspecialty and the Brain Trauma Foundation are privileged to work with and learn from our colleagues in the military, with the goal of translating their insights to civilian contexts and improving head injury outcomes for everyone.”
As a result of recent conflicts around the world, head injury has taken on a new urgency, Dr. Hawryluk says. “There is enhanced recognition of the need to serve injured soldiers in new ways,” he notes, “as head injury is a critical wounding mechanism in modern military conflicts.”
Advertisement
He explains that the very nature of combat head injuries has evolved, extending beyond traditional concerns like shrapnel wounds. For example, the widespread use of body armor, while protective against projectile impacts to the torso, can paradoxically exacerbate brain injury, as body armor can act like a plunger, transmitting the force of a blast wave upwards, potentially rupturing blood vessels in the brain. This broadened understanding of injury mechanisms underscores the need for specialized knowledge and tailored treatment strategies in military settings, Dr. Hawryluk notes.
In response to these evolving challenges and a need for contemporary guidance, the BTF will soon publish its first comprehensive penetrating head injury guidelines, with Dr. Hawryluk as one of the effort’s leaders. This initiative comes at a crucial time, with early draft versions of these guidelines already being used in active conflict zones such as Gaza and Ukraine for the past couple of years. Formal publication is expected this summer or fall.
The new guidelines — which reflect consensus among 31 global experts, over half with military backgrounds — have several key tenets. Perhaps most significant is the strong discouragement of nihilism in the face of penetrating head injury. “These guidelines challenge the outdated notion that such injuries invariably lead to poor outcomes,” Dr. Hawryluk says. “Instead, they stress the military’s observation that aggressive management can lead to surprisingly good results in some cases, leading to an emphasis on early surgery for debridement and CSF leak prevention.” Additionally, the guidelines underscore that penetrating head injury presents a fundamentally different clinical picture compared with blunt head injury, with complex vascular injury being a particularly salient feature.
Advertisement
“Another major tenet of the new guidelines is an imperative for physicians to actively screen for and aggressively treat these complex vascular lesions,” says Dr. Hawryluk. He also notes that penetrating injuries are not always immediately apparent, particularly in chaotic environments such as a battlefield where the point of entry may be subtle or the mechanism of injury not immediately clear. In response, the guidelines advocate a high index of suspicion for penetrating injury and recommend CT as the most reliable screening modality. While X-ray can play a role in identifying metal fragments, the guidelines note that CT provides superior anatomic detail.
Dr. Hawryluk identifies prevention of CSF leaks as an additional priority from the guidelines, as such leaks can serve as pathways for devastating brain infections. Given that large skull defects from penetrating trauma do not heal spontaneously, the guidelines stress the need to employ various techniques to seal these holes, including use of autologous or even foreign materials. In contrast to the paucity of high-level evidence for most recommendations in the field of head injury, Dr. Hawryluk notes that active prevention of CSF leaks received a rare Level 2 recommendation, reflecting moderately strong evidentiary support.
Development of the penetrating head injury guidelines served as inspiration for a formal collaboration between the BTF and the U.S. Department of Defense’s Military Traumatic Brain Injury Initiative, announced in April 2024. The success of the guidelines prompted interest from the military in development of more clinical practice guidelines to promote swifter translation of care advances to soldiers. The current five-year partnership has enabled the BTF to overcome the challenges of intermittent grant cycles and significantly accelerate its guideline production, Dr. Hawryluk says.
Advertisement
He notes that the collaboration is now developing guidelines for the following:
“Ever since the Brain Trauma Foundation’s first guideline was published in 1996,” Dr. Hawryluk observes, “people have said that these guidelines are really good for a well-resourced American hospital but that many care environments in America and around the world are not well resourced yet still need to treat head injuries.” Such observations led to calls for resource-stratified guidelines, but these arguments were tempered by concerns that providing such guidelines might lead hospitals to underinvest in their neurotrauma care capabilities even if they could afford to fund optimally resourced care.
Advertisement
In recent years, however, the BTF has come to recognize the demand for resource-stratified guidelines as an imperative, Dr. Hawryluk notes. For instance, acknowledging that their “best-case scenario” guidelines might not be directly applicable in resource-limited settings, the BTF is incorporating resource stratification into the upcoming fifth edition of its adult coma guidelines. This will provide tailored recommendations for environments lacking advanced resources.
“We want to address how to provide the best possible care if CT imaging, ICU resources and brain pressure monitoring aren’t available and a neurosurgeon isn’t accessible,” Dr. Hawryluk explains.
The shift toward resource-stratified guidance has dovetailed with significant advancements in technology, particularly in noninvasive diagnostic modalities for both mild and severe head injuries. Such technologies are being actively evaluated for inclusion in the BTF’s forthcoming guidelines for austere care environments, Dr. Hawryluk says. He identifies several promising modalities:
“In the forthcoming guidelines, we say that while the gold standard of CT evaluation is still best, these technologies are rapidly getting much better and can be used when CT isn’t available,” Dr. Hawryluk says. “More than one of these modalities should be used whenever possible, with the goal of concordance among them.” He adds that the new guidelines for austere environments will be the first to recommend a definitive threshold for treatment based on optic nerve sheath ultrasound, with a diameter exceeding 6 mm suggesting elevated intracranial pressure that warrants intervention.
Even as Dr. Hawryluk supports the BTF’s move to tailor care recommendations to a variety of care environments, he emphasizes the need for well-resourced neurotrauma care to be made available as broadly as possible. “As Cleveland Clinic Akron General is a Level I Trauma Center, I see the value of such care every day,” he says. Such resourcing can take the form of anything from ready availability of portable CT scanners to clinical trial access to newly approved “headbands” for monitoring intracranial dynamics.
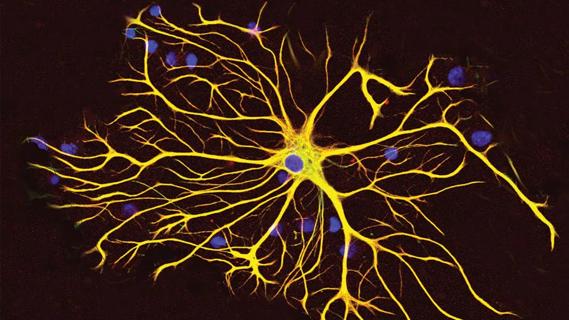
Optimal resourcing also makes possible research into fundamental but only recently recognized aspects of human brain injury, such as cerebrovascular autoregulatory processes and cortical spreading depressions/depolarizations. Dr. Hawryluk’s own research into these and other phenomena will be bolstered by the recent addition of a distinguished physicist, Mark Krasberg, PhD, to his research team. “There is incredible value to bringing together accomplished people with very different skill sets to solve problems,” Dr. Hawryluk says. “Dr. Krasberg ran the IceCube neutrino detector on Antarctica and was involved in the discovery of the top quark. The addition of Dr. Krasberg’s high-end physics work to our neuromonitoring program opens up a lot of possibilities for research and patient care that are not available elsewhere.”
Advertisement
Q&A with Brain Trauma Foundation guideline architect Gregory Hawryluk, MD, PhD
GFAP elevation may signal increased risk of progressive regional atrophy, cognitive decline

Care guidelines have been crucial to progress in TBI care over the past 25 years

An expert talks through the benefits, limits and unresolved questions of an evolving technology

Recommendations on identifying and managing neurodevelopmental and related challenges

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape