A partnership between a skull-base rhinologist and a neurosurgeon has helped advance a technique with favorable outcomes and minimal postoperative morbidity

Surgeons at Cleveland Clinic have published the world’s largest single-center experience to date on an innovative endoscopic endonasal approach to removing or sampling benign intraconal orbital tumors. The research appears in Laryngoscope.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Even when benign, tumors that arise in the deepest part of the eye socket, the intraconal space, can still cause vision loss or neurologic deficit if not removed. But accessing these tumors has been challenging for reasons related to both anatomy and expertise, says Raj Sindwani, MD, Co-Director of the Minimally Invasive Cranial Base and Pituitary Surgery Program at Cleveland Clinic.
“The intraconal space is kind of a no-man’s land. It’s not a place that ocular surgeons can access easily, because the eye is a bony box. In many cases, they can’t move the globe and other contents out of the way enough to see to the back of the eye well enough to carefully take the entire tumor out,” Dr. Sindwani explains.
This location isn’t traditionally in the wheelhouse of neurosurgeons either, since it’s not in the brain, or of otolaryngologists, since it’s not in the ear, nose, or throat. Thus, patients are often told that tumors in the intraconal space are inoperable.
“If you don’t offer surgery, you’re left either watching the tumor or trying to irradiate some of them. These are the same considerations on the intracranial side as well, where we commonly find tumors pressing on the optic nerve. Some tumors respond to radiation, but many do not. The experience of removing tumors away from the optic nerve through cranial procedures serves us well for the removal through an endonasal approach. Because these tumors are close to the optic nerve, radiation treatment may be worse than the disease,” notes Pablo F. Recinos, MD.
Advertisement
About a decade ago, Dr. Sindwani, a rhinologist and skull-base surgeon, teamed up with the Neurological Institute’s endoscopically-trained neurosurgeon, Dr. Recinos, and together they formed the Minimally Invasive Cranial Base and Pituitary Surgery Program at Cleveland Clinic. They attempted to use the same two-surgeon, multi-handed endoscopic endonasal approach they had long used for brain tumors and other skull-based procedures for intraconal orbital tumors.
“Dr. Recinos and I operate together, simultaneously, with multiple hands and multiple instruments going in and out of both nostrils to be able to offer the optimal amount of control and precision in taking tumors out of very critical areas. We felt ourselves well-positioned and uniquely qualified to expand our expertise to include orbital surgery, especially to these deep spaces of the eye,” Dr. Sindwani explains.
Surgical principles of skull-base surgery, including minimizing retraction on the brain and creating a direct line to tumors between the nose and the brain, are similar to operating on the eye, in terms of minimizing traction on the globe and optic nerve and using a direct approach to the tumor through the nose, he points out.
Cleveland Clinic’s armamentarium also includes endoscopic OR suites equipped with navigation systems, specialized angled-endoscopes and other tools to enable the optimization of outcomes.
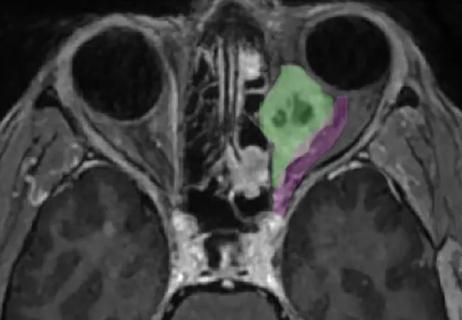
The intraconal procedure involves a septectomy and orbital decompression of the layers between the nose and the orbit, followed by opening the periorbita and exposing the orbital contents. “Importantly, we use the corridor between the medial rectus muscle and the inferior rectus muscle. That’s the safest way to get into the deep space. Using multiple instruments, we move the medial rectus muscle up and follow underneath it to get into the intraconal space of the orbit,” explains Dr. Recinos.
Advertisement
Using navigation and specially designed skull-base instruments, Dr. Sindwani and Dr. Recinos gently dissect the tumor from any attachment that it might have coercing it away from critical structures including the optic nerve and small blood vessels of the orbit.
Since visualization is at an angle, they use a technique called “hugging the capsule” of the tumor, meaning that “we stay extremely close to the surface of it and come all the way around 360 degrees so that we can gently pluck it away from those critical structures. You can’t be too heavy-handed about taking it out. The technique is gentle, blunt dissection.”
The 13 men and seven women in the published series underwent endoscopic endonasal procedures between January 2014 and December 2021. All had lesions limited to the medial intraconal space, detected following visual symptoms (visual loss, diplopia and/or orbital pain) in 16 and incidentally found in four. Half of the procedures were complete resections through two nostrils and the other half, when malignancy was suspected, were biopsies taken through a single nostril approach.
The tumor types included six cavernous hemangiomas, four schwannomas, four lymphomas, two inflammatory pseudotumors, two chronic invasive fungal sinusitis and two metastatic diseases.
Drs. Sindwani and Recinos performed all 20 procedures using the multi-handed approach to the medial intraconal space through the endonasal corridor between the medial and inferior rectus muscles. They were able to totally resect nine of the 10 benign lesions and achieve pathologic diagnosis in all ten of the biopsies.
Advertisement
Interestingly, no subsequent orbital reconstruction was required. “That partition forms automatically by the body to separate out the eye from the nasal cavity, so there’s very minimal reconstruction needed in the vast majority of cases in our experience. It speaks to the healing ability of the body and how it naturally wants to separate out those spaces,” Dr. Sindwani notes.
There were no visual changes following the 10 biopsies. Among the 10 planned resection cases, visual acuity returned to normal in eight, with no change in the other two. All of the resection patients experienced postoperative diplopia, but this resolved by three months in nine patients, while the tenth was lost to follow-up.
This temporary diplopia is to be expected, Dr. Sindwani says. “When we’re done, the muscles have a very changed anatomy and, until the new periorbita forms, the muscles can’t pull and tug on the eyeball to move it in a coordinated way with the other eye. Once the healing starts, the coordination of movement from one globe to the other globe can happen, but this takes time.”
This should be discussed openly with patients before surgery, he says. “We warn everybody that for the first couple months postop they might have severe double vision (diplopia). We even discuss with all patients that they might need further surgery down the road if the diplopia doesn’t clear up, but in the large majority of cases it does resolve over a few months.”
The primary goal of the surgery has been to prevent further vision loss, so the improvement in visual acuity in some patients has been a bit of a surprise, Dr. Recinos notes. “There’s no guarantee. Sometimes the tumor has been pressing for so long that the nerve is damaged, although in our experience some patients have had dramatic improvements in vision even when it was down for some time. We can’t know this in advance, however.”
Advertisement
Over time, Dr. Sindwani and Dr. Recinos have become more efficient at performing this procedure, and sometimes an ophthalmologic surgeon assists in cases that are closer to the globe. “As with all procedures, there is definitely a learning curve, and it’s a very confined space so you want to make sure you have the right team, the right tools and the right infrastructure to get the best outcomes. We’re very fortunate at Cleveland Clinic to have all those things available.” Dr. Sindwani, recently published a textbook on “Endoscopic Surgery of the Orbit” (Elsevier, 2021) and as Editor-in-Chief of the American Journal of Rhinology and Allergy, is now working on a special issue on endoscopic orbital surgery, planned for publication in 2024. This new work, he explains, is “the next iteration of the progression of everything we’ve learned over the past few decades as a skull base team.”
Advertisement

Registry data highlight visual gains in patients with legal blindness

Study is first to show reduction in autoimmune disease with the common diabetes and obesity drugs

It’s the first step toward reliable screening with your smartphone

Fixational eye movement is similar in left and right eyes of people with normal vision

Oral medication may have potential to preserve vision and shrink tumors prior to surgery or radiation

A new online calculator can determine probability of melanoma

Only 33% of patients have long-term improvement after treatment
Novel collaborative approach helps patient avoid orbital exenteration