Patients with diabetic eye disease are most affected
Undertreatment is a real concern in patients who need regular intravitreal anti-VEGF or steroid injections to help control diabetic macular edema (DME), proliferative diabetic retinopathy (PDR), neovascular age-related macular degeneration (nAMD) or retinal vein occlusion (RVO). Depending on extent of disease, injections usually need to be administered every four to 12 weeks.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
While numerous studies have explored treatment burden in this population and the consequences of delayed care, the shutdown due to the COVID-19 pandemic presented a unique research opportunity.
“During the pandemic, we faced an unprecedented situation in which many patient appointments were canceled or delayed,” says Aleksandra Rachitskaya, MD, a retinal specialist at Cleveland Clinic’s Cole Eye Institute. “That allowed us a relatively controlled environment in which we could study a large number of people who skipped or postponed intravitreal injections at the same time.”
Dr. Rachitskaya led a team in studying the effect of delayed care on visual acuity in these patients. Their results were published in Ophthalmology Retina. The team found that, when compared to patients who completed their scheduled visits, patients who missed an injection had greater vision loss. Those with DME, PDR (or both) or RVO recorded the most vision loss; those with nAMD recorded the least.
More than 1,000 adult patients with DME, PDR, nAMD or RVO (N = 1,041) were included in the retrospective study. All had been scheduled to see an ophthalmologist at Cole Eye Institute during the COVID-19 shutdown, March 14, 2020, to May 4, 2020. All had received an intravitreal injection within the previous 12 weeks.
A chart review revealed that during the shutdown:
The average delay in care of patients who canceled or otherwise missed their visit was 5.34 weeks. During their next visit, their recorded visual acuity was worse than that of patients who completed a scheduled visit.
Advertisement
“These results were not what we expected,” says Dr. Rachitskaya. “In AMD in general, progression to wet type happens rapidly, while DME progresses more slowly. Thus, we anticipated that one missed injection would be more detrimental in nAMD and not as detrimental in DME, but we saw the opposite.”
The big question is if vision returns to baseline when treatment resumes, she says. The research team currently is studying long-term effects, including taking a closer look at the reason for vision loss.
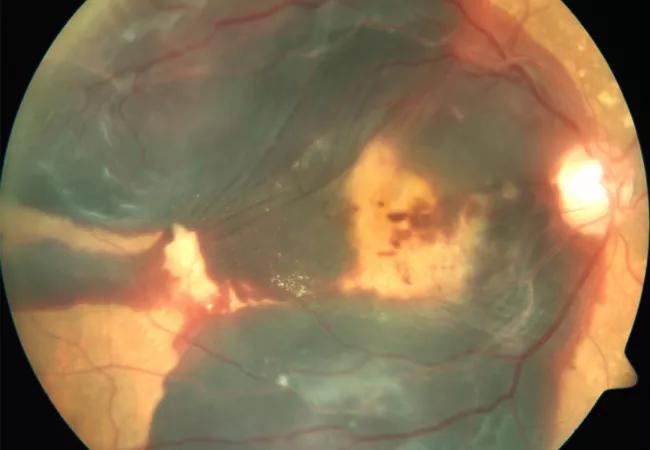
“In some cases the vision loss might be reversible, and in other cases it is not,” says Cole Eye Institute ophthalmologist Rishi P. Singh, MD, a co-author of the study. “Even small episodes of fluid accumulation can cause irreparable damage to the retina and vision. Or there may be more advanced complications, such as bleeding in the eye, retinal detachment or abnormal revascularization. One-year data is important for us to further determine the effects of short-term care delays on long-term prognosis.”
Beyond visual acuity, researchers reported that patients who canceled a visit tended to be older. Patients who were no-shows tended to be younger and male, have lower baseline vision and have diabetes.
“In a sense, no-show demographics helped us make a ‘composite sketch’ of one of our most vulnerable patient populations,” says Dr. Rachitskaya. “Younger men with diabetes may be at a higher risk of missing appointments and not getting the treatment they need. Providers need to be aware and help these patients prevent gaps in care.”
Advertisement
Regardless of demographics, even a short delay in care — five weeks in this study — can result in patients’ vision loss.
“This data may help providers reinforce compliance with patients,” says Dr. Rachitskaya. “With a fuller understanding of the disease, we can better educate patients about what to expect if they miss even one injection.”
Advertisement
Advertisement

Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma

Registry data highlight visual gains in patients with legal blindness

Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence

A look at emerging technology shaping retina surgery

A primer on MIGS methods and devices

7 keys to success for comprehensive ophthalmologists

Study is first to show reduction in autoimmune disease with the common diabetes and obesity drugs

Treatment options range from tetracycline injections to fat repositioning and cheek lift