Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units
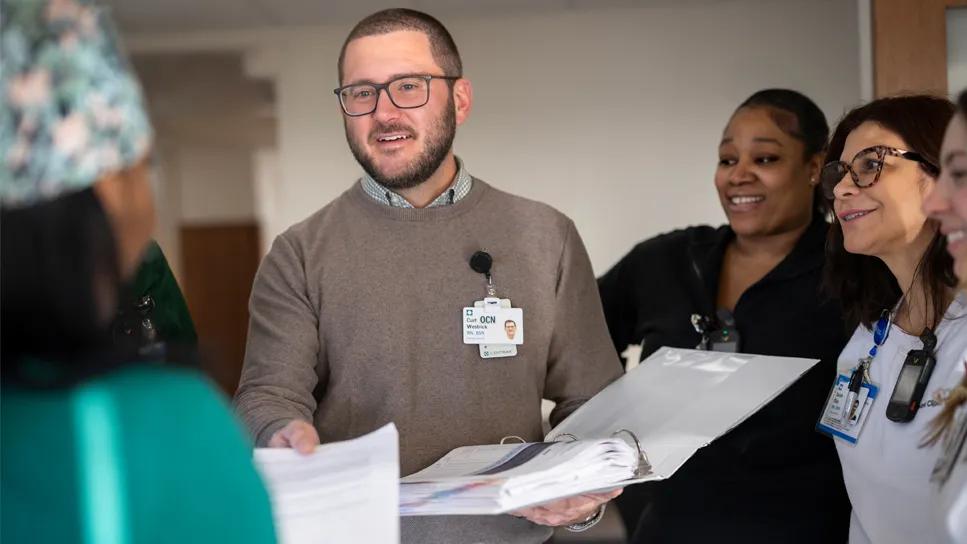
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/de3aab83-2876-4377-ba9e-bf360ceb5ce3/nurse-manager-with-team-bmt-and-leukemia)
Oncology nurse
Caring for patients with blood cancers is a complex endeavor. Advances in clinical care also present new opportunities for caregivers to consider ways to improve patient outcomes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Curt Westrick, BSN, RN, OCN, is a clinical nurse manager who's led many care improvements at Cleveland Clinic Cancer Institute. As the nurse manager for both the Leukemia and the Bone Marrow Transplant (BMT) units, Westrick supervises caregivers providing specialized nursing care. He recently shared learnings gained that helped to improve outcomes for patients and providers.
Many patients in the Leukemia and BMT units are dependent on blood products and electrolyte therapy. To help patients sleep longer at night, the Leukemia team trialed moving blood draws from 4 a.m. until midnight. That way if the results show the patient doesn't need a blood transfusion or electrolyte therapy, they can sleep through until the next set of vitals or until PO medications are scheduled. Surveys collected by unit leadership showed that patients found this a net positive in terms of their ability to get a restful sleep.
Aids also now coordinate taking vitals at the same time as blood draws to reduce the number of interruptions for patients.
In looking at sleep patterns, Westrick and his team also found that patients were receiving premedication such as Benadryl for blood transfusions during the day, and that could disrupt their circadian rhythm. By administering blood earlier in the night, these doses could be given earlier to help patients get a full night's sleep.
Administering more blood products and electrolytes during the night shift led to balancing workloads between night and day shifts. With 24-hour care, issues can spill over from one shift to the next, putting pressure on the team when starting their shift.
Advertisement
Westrick arranged for some tasks such as administering blood transfusions and electrolyte replacement therapy to be performed by night shift nurses. This allowed day shift nurses to prioritize starting their day by seeing their sickest patients first instead of needing to complete a time-sensitive task. This approach allowed nurses to address emerging needs such as implementing new orders, responding to changes in patient conditions and discharging patients.
In the leukemia and BMT population, most patients have central lines, which are susceptible to infections. The hospital was looking for ways to reduce central line-associated bloodstream infections (CLABSIs), which are an NDNQI quality metric. As part of its process confirmation, the nursing team conducts daily process checks via a 13-point central line maintenance assessment form.
The team created a workflow to ensure process confirmation with the RN at the bedside during the shift change. Any deficiencies identified are recorded and addressed on the spot, with findings shared with nursing leadership via the process confirmation website.
Additionally, in evaluating the central line assessment forms, the nursing team found that despite education, many patients were not following chlorhexidine (CHG) interventions properly. These interventions are helpful for infection protection. To solve this issue, the team created signage for patients' bathrooms with clear instructions on completing CHG baths.
By confirming their process with central line maintenance and educating patients on CHG use, the team experienced seven months with no CLABSIs.
Advertisement
Currently, the team is working on an initiative to further reduce fall risks. One method has been to screen for delirium using the Brief Confusion Assessment Method (bCAM) tool, with each change in RN caregiver at a minimum of every 12 hours. This tool is excellent at establishing a mental baseline and identifying hypoactive delirium, which is highly underdiagnosed in hospital settings. This systematic approach to screening for delirium has empowered RNS to activate interventions such as using the bed alarm on patients who may not have previously been understood to be delirious. Since doing so, the unit had 35 days with no falls.
They've also discovered there are subtle signs to watch for that indicate a patient may be experiencing delirium. "I've learned that if a patient is being overly polite, it can be a sign of hypoactive delirium," explains Westrick. "The rationale is that they're trying to end the interaction as quickly as possible because they don't understand why you are in their room or because they are experiencing paranoia. Sharing these learnings with my team will hopefully help make things safer for patients in the hospital."
"We're supporting patients and their loved ones who are adjusting to a life-changing event," says Westrick. "Each interaction is an opportunity to get to know a patient better as an individual. When we do quality rounds, those are meant to check on safety and related issues, but I always take a moment to connect with the person, read the room and see if they're open to an interaction. If so, I'll stay and chat with them a bit longer. Even small things like asking about their day or just being respectful that the hospital room is their space can make a big difference."
Advertisement
Nursing can be quite stressful in these units. Patients may become very sick, and the demands of the job put a lot of pressure on nurses to prioritize care needs. "One of the recommendations we received recently was to start doing decompression huddles," explains Westrick. "For example, if we have a patient who's challenging or who has been escalating, we'll have a decompression huddle after the fact.
This increases empathy and raises awareness of how the situation affected everyone. It's built around the concept of giving people a safe space to talk out stressors they're experiencing. It's been helpful so people aren't taking stress home with them, providing a way to recharge and come back ready to go the next day."
Westrick also pays a good deal of attention to ensuring his team has the tools they need to perform their job, while providing incentives to perform in line with Cleveland Clinic's expected service behaviors. Performance ratings are tied to subjective quality metrics such as administering antibiotics within one hour of being ordered by the physician, timely flowsheet documentation and the number of CHG interventions documented, to name a few.
As they look to the future, the nursing team continues to use strategic planning and process improvements to enhance team performance and patient experiences.
Advertisement
Advertisement
Making a difference by putting empathy into action
Automating routine medical coding tasks removes unnecessary barriers
Input from these central stakeholders is leading us to design for healing and hope
Initiative ensures patients leave the hospital with clean, dry clothing
Palliative and Supportive Care Teams offer comprehensive care to improve the lives of patients facing cancer
Leadership role offers a way to improve the entire visit
Cleveland Clinic’s new dedicated program offers nuanced care for a newly recognized cardiovascular risk factor
An unexpected health scare provides a potent reminder of what patients need most from their caregivers