Updated meta-analysis supports personalizing antiplatelet strategies
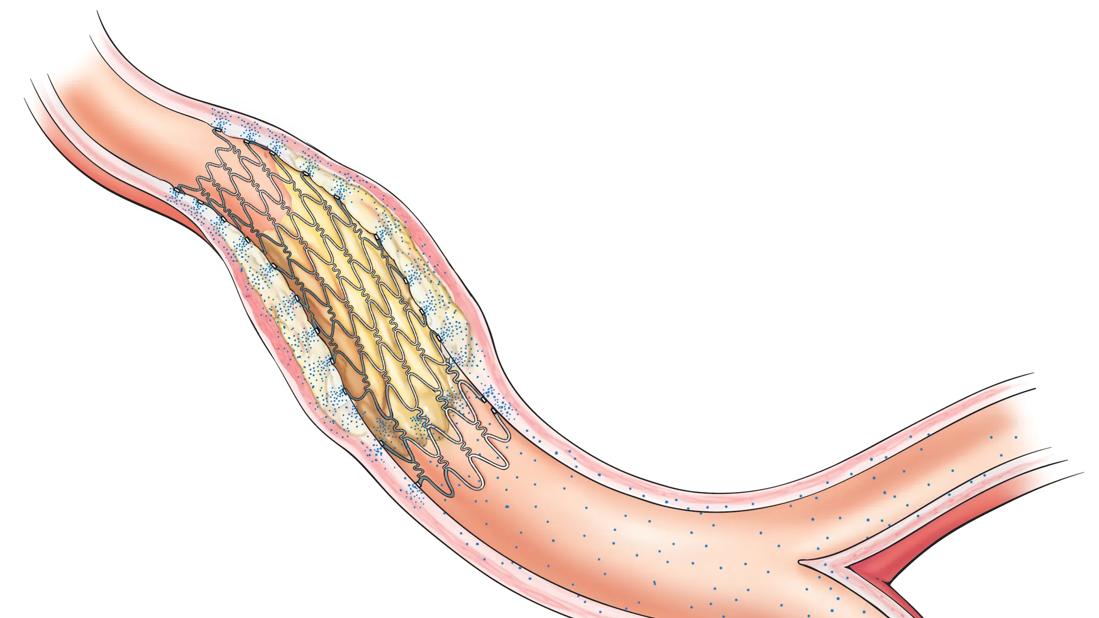
Use of dual antiplatelet therapy (DAPT) for more than 12 months after percutaneous coronary intervention (PCI) with drug-eluting stents (DES) is associated with a lower rate of myocardial infarction (MI) than shorter periods of DAPT use. However, the benefit comes at a cost — a higher risk of major bleeding. While shorter DAPT strategies confer similar ischemic protection to each other, DAPT for less than six months followed by P2Y12 inhibitor monotherapy entails the lowest risk of bleeding events.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Those are the primary conclusions of a large meta-analysis of randomized controlled trials recently published online in Circulation by a multi-institutional team of researchers.
“Our analysis suggests that there is not a single best antiplatelet strategy for all patients following PCI,” says study co-author Ankur Kalra, MD, a Cleveland Clinic cardiologist. “Providers need to consider each patient’s risk of ischemia and bleeding to determine the optimal DAPT intensity and duration.”
Recommendations concerning DAPT after PCI continue to evolve as more evidence emerges. Guidelines from the European Society of Cardiology (2017) and the American College of Cardiology/American Heart Association (2016) offer somewhat different recommendations depending on bleeding risk, stent type and presence of acute coronary syndrome.
The European and American guidelines were based on 15 randomized controlled trials; since then, additional clinical trials have been published.
The new meta-analysis analyzed 24 randomized controlled trials comprising 79,073 patients and with a median follow-up of 18 months. Fourteen of the trials reported outcomes in patients with acute coronary syndrome.
The following strategies after PCI with DES were compared:
The primary endpoints were MI and major bleeding.
The analysis revealed the following outcomes:
Advertisement
Notably, none of the strategies was associated with significant differences in either cardiovascular or overall mortality.
The investigators point out several study limitations, including that only one-third of the trials were powered to test superiority of different DAPT strategies (the others were powered for noninferiority). Also, studies differed in design and baseline health status of patients, with relatively few patients having acute coronary syndrome.
Still, Dr. Kalra notes that this meta-analysis extends findings from previous analyses by incorporating more recent clinical trials. He highlights the following key takeaways from the new study:
“This study can reassure physicians that for many patients, a short-term DAPT course followed by P2Y12 inhibitor monotherapy is reasonable,” concludes study co-author Samir Kapadia, MD, Chair of Cardiovascular Medicine at Cleveland Clinic. “But high cardiovascular and low bleeding risks could tip the decision to an extended DAPT strategy.”
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more