Case-control study assesses risk factors that play a role in tumor necrosis factor-α inhibitor-induced psoriasis

By Anthony Fernandez, MD, PhD, and Elaine Husni, MD, MPH
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
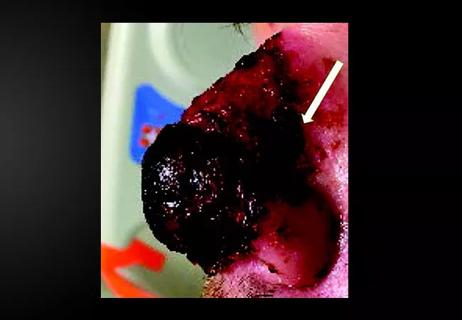
Although are more than 500 reported cases of tumor necrosis factor-α inhibitor (TNFI) -induced psoriasis and over 15 years of experience with the condition, our understanding of its pathogenesis remains incomplete. The symptoms of TNFI psoriasis can be severe enough to prompt discontinuation of the treatment, even if it has achieved disease control for the underlying condition. Thus, it is important for rheumatologists and dermatologists to gain an understanding of the risk factors associated with TNFI psoriasis as they consider the risks and benefits of this treatment.
To that end, we recently concluded a case-control study to identify underlying risk factors and triggers associated with the onset of TNFI psoriasis. The study was published in the Journal of the American Academy of Dermatology.1
Our team reviewed details in the electronic medical records of 97 patients with TNFI psoriasis treated at our institution between 2003 and 2013. These records were compared with matched controls who were treated with TNFIs but did not develop TNFI psoriasis between 2003 and 2015. In these groups, the average age at initiation of TNFI therapy was 41 years and 73% of patients were women. The patients who developed TNFI psoriasis were exposed to one of the following TNFIs: adalimumab (33%), etanercept (18%) and infliximab (50%).
For each patient cohort, we went back 6 months prior to TNFI treatment initiation, looking for information about potential risk factors. Risk factors explored were categorized as serologic abnormalities (i.e., antinuclear antibody, white blood count, peripheral eosinophilia), acute events (skin or soft tissue infection, upper respiratory infection, acute psychological stressor, gastroenteritis) and social factors (family history of psoriasis, history of using alcohol, tobacco or illicit drugs).
Advertisement
This case analysis identified family history of psoriasis (24% in the TNFI psoriasis group vs 3% in the control group, P = .0003) and acute psychological stressors (96% vs 54%; P = .0009) as risk factors associated with TNFI psoriasis. The only other potential risk factor we identified was tobacco use – and that was only a marginal association (33% vs. 22%; P = .10). All three associations were confirmed after multiple imputation analysis, with odds ratios of 5.54 for family history of psoriasis, 3.14 for acute psychological stressors and 1.76 for tobacco use. Our findings are consistent with previously published studies.
Which patients will develop TNFI-induced psoriasis – and why – have remained a mystery. Patients can develop TNFI psoriasis at any point during treatment, with cases reported as early as 1 week after initiation to several years following initiation. This temporal variation, along with a low incidence of this reaction in patients taking TNFIs (1-3 per 1,000 years),2,3 suggest that underlying risk factors play a role in the onset of TNFI psoriasis.
Our study adds to the existing literature suggesting that genetics, psychological stress and (perhaps) tobacco are associated with the development of TNFI-induced psoriasis. Although we had hoped to identify specific triggers, we only identified acute psychological stress as a trigger that might explain some of the temporal variability. Future studies are needed to confirm these associations and explore external triggers of TNFI psoriasis.
Advertisement
Advertisement
Advertisement

Family history may eclipse sun exposure in some cases

Consider secondary syphilis in the differential of annular lesions

Persistent rectal pain leads to diffuse pustules

Two cases — both tremendously different in their level of complexity — illustrate the core principles of nasal reconstruction
Stress and immunosuppression can trigger reactivation of latent virus

Low-dose, monitored prescription therapy demonstrates success

Antioxidants, barrier-enhancing agents can improve thinning hair