Injection pharyngoplasty could be lower-risk intervention
Injection pharyngoplasty, a fat grafting procedure, has historically been performed in a pediatric setting, frequently to augment cleft palate surgery. In a recent investigation, Cleveland Clinic otolaryngologists examined the safety and utility of injection pharyngoplasty in a less understood clinical setting — adults with mild to moderate velopharyngeal insufficiency (VPI). They reported their findings in the Annals of Otology, Rhinology & Laryngology.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
VPI is characterized by a structural defect in the soft palate and pharynx that limits the complete closure of the velopharyngeal port. Patients with VPI may have hypernasal speech and difficulty making certain sounds, explains Paul Bryson, MD, Director of Cleveland Clinic’s Voice Center and Section Head of Laryngology in the Head & Neck Institute. Complete or near closure of the velopharyngeal port allows patients to speak and swallow without refluxing air, foods or liquids into their nasal cavities.
While VPI is more common in children and is often associated with congenital conditions (like a cleft palate) or after surgical procedures (like removal of the tonsils or adenoids), it is not a uniquely pediatric condition. Among other potential causes, VPI in adult patients can be the result of oral surgery, radiation or a neurologic condition. It can also happen naturally due to age-related atrophy of the nasopharynx.
“We hoped to better understand the clinical value of using injection pharyngoplasty in adult patients with VPI. There isn’t an optimal standard of care for this patient population,” says Dr. Bryson. “Often, they are either referred to speech pathology or are treated surgically with local tissue flaps, which can be a complex procedure.” Understandably, some patients will opt to go without treatment altogether rather than undergoing major reconstructive surgery.
As for the procedure itself, surgeons harvest subcutaneous fat from a small 2 cm incision in the abdomen. The fat is processed and injected into the pharynx under endoscopic guidance. A range of 3 to 6 cc of fat is injected into the posterior pharyngeal wall where the soft palate has incomplete closure. Dr. Bryson cautions that the injection should be placed within the submucosa and superior constrictor — not any deeper than the retropharyngeal fascia and must be anterior to alar fascia (Figure).
Advertisement
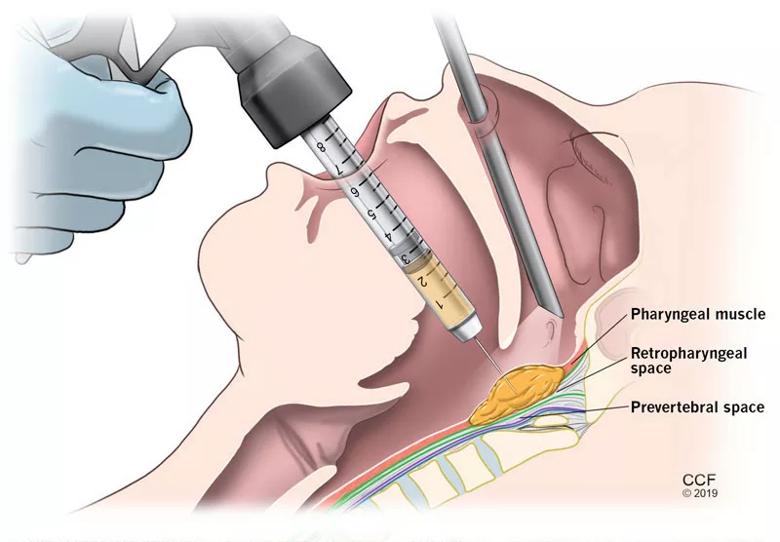
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1e04578d-297c-484f-a3be-05af092af026/19-ENT-5075-NeckIllustrationWfat-inset-800x556_jpg)
Figure. Transoral injection of fat with nasal endoscopic guidance
To better understand the effect of injection pharyngoplasty as an intervention for adult patients with VPI, the physicians examined outcomes in 11 patients with a mean age of 41, who received the procedure from 2012 to 2018. Symptoms were reported before and after the procedure, with symptomatic improvement noted by the treating physician on a scale of 0 (none) to 4 (complete).
The mean subjective improvements for rhinophonia and dysphagia were moderate with an increase in postoperative scoring at 2.3 and 2.0, respectively. Dynamic evaluation of VPI by flexible nasopharyngoscopy also demonstrated a mean improvement of 3.0 (i.e. near-complete). Two patients experienced minor postoperative complications that resolved without issue but, overall, there were no major complications to report.
Kevin Contrera, MD, an otolaryngology resident at Cleveland Clinic and the study’s first author, notes that the findings demonstrate that the procedure is safe and effective. “Although nearly half of patients required subsequent intervention — another fat injection or surgical pharyngoplasty — almost all patients obtained at least some degree of benefit based on their speech and their endoscopic evaluations,” he says. Anecdotally, the patients who required follow-up intervention were the ones who presented with worse outcomes, the researchers say.
Dr. Bryson notes that future studies may focus on a larger sample size of patients and a comparative look at injection pharyngoplasty versus surgical pharyngoplasty; however, he says, these findings demonstrate the safety and utility of injection pharyngoplasty for this patient population. “While this remains an area of investigation, we are heartened that this seems to be a viable, minimally invasive approach for adult patients with mild to moderate VPI.”
Advertisement
Advertisement

Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor

Case study illustrates the potential of a dual-subspecialist approach

Evidence-based recommendations for balancing cancer control with quality of life

Study shows no negative impact for individuals with better contralateral ear performance

HNS device offers new solution for those struggling with CPAP

Patient with cerebral palsy undergoes life-saving tumor resection

Specialists are increasingly relying on otolaryngologists for evaluation and treatment of the complex condition

Detailed surgical process uncovers extensive middle ear damage causing severe pain and pressure.