Novel TAVR deployment technique improves outcomes without compromising safety
Among patients undergoing transfemoral transcatheter aortic valve replacement (TAVR), implanting the balloon-expandable Edwards SAPIEN 3 valve with higher placement — in a position just 1.5 mm under the noncoronary cusp — led to greater than 50% reductions in rates of conduction abnormalities and 30-day permanent pacemaker implantation compared with conventional valve deployment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
So found a study comparing outcomes in more than 1,000 patients who underwent TAVR at Cleveland Clinic before or after transition to the new deployment method. The results were published online January 12 in Circulation: Cardiovascular Interventions.
“As TAVR use increases among patients with longer life expectancy, finding new ways to improve the procedure is especially important,” says the study’s senior author, Samir Kapadia, MD, Chair of Cardiovascular Medicine at Cleveland Clinic. “We found that the high deployment technique for aortic valve implantation appears to be a significant step forward, as outcomes improved without compromising procedural safety or valve hemodynamics.”
Although TAVR is considered a safe alternative to surgery for patients with severe, symptomatic aortic valve stenosis, it is well known to be associated with risk of new-onset conduction disturbances and permanent pacemaker requirement. Conventional deployment of the balloon-expandable SAPIEN 3 valve results in a ratio of valve frame in the aorta to left ventricular outflow tract of 70:30 or 80:20, a level that may put pressure on conduction tissue at and below the annular plane (see Figure).
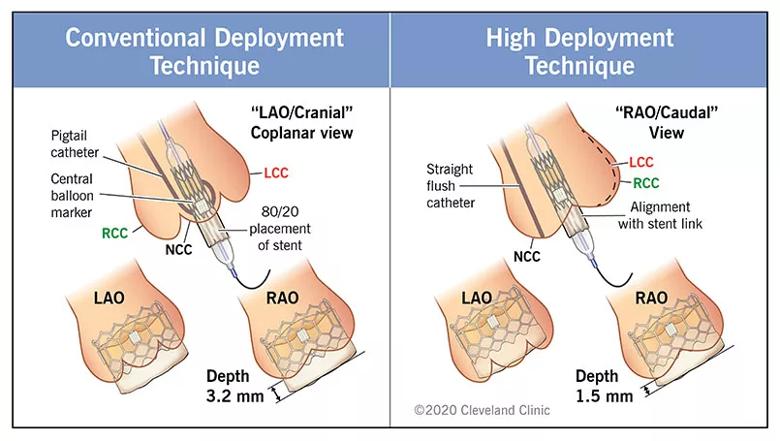
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ebdafbd1-df5b-4d14-8046-62dd6f8637ed/21-HVI-2035428_conventional-vs-high-deployment-SAPIEN-3-valve_inset_jpg)
Figure. Differences between the conventional and high deployment techniques for placing the SAPIEN 3 valve. LAO = left anterior oblique; RAO = right anterior oblique; LCC = left coronary cusp; RCC = right coronary cusp; NCC = noncoronary cusp.
In April 2017, Cleveland Clinic TAVR operators started to use a novel high deployment technique to achieve higher implantation of the SAPIEN 3 valve, with the goal of reducing impairment of the conduction system. From January 2018 on, all TAVR procedures using the SAPIEN 3 valve performed at the institution employed the high deployment technique.
Advertisement
All consecutive patients who underwent transfemoral TAVR with the SAPIEN 3 valve at Cleveland Clinic between April 2015 and December 2018 were included in this retrospective study. Of the 1,028 total patients, 622 (60.5%) underwent the conventional deployment technique and 406 (39.5%) underwent the high deployment technique. Overall, the median patient age was 82.7 years, and the median Society of Thoracic Surgeons risk score was 4.9 (interquartile range, 3.6-7.3).
Patients with a preexisting permanent pacemaker were included in the overall analysis but were excluded from the endpoint analyses of the need for a new permanent pacemaker and new onset of conduction abnormalities.
Key changes observed with adoption of the high deployment technique included the following:
Advertisement
Additional key outcomes were similar between the two techniques:
The study report describes the technique for achieving high valve deployment. The technique was applied to all types of aortic root anatomy, in different angulations and with varying degrees of the valve being centered in the annulus. The authors share the following tips:
Advertisement
“As a result of our experience, we recommend that high deployment of the SAPIEN 3 valve be adopted to decrease implantation depth and improve patient outcomes after TAVR,” concludes Dr. Kapadia.
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more