New Cleveland Clinic data challenge traditional size thresholds for surgical intervention
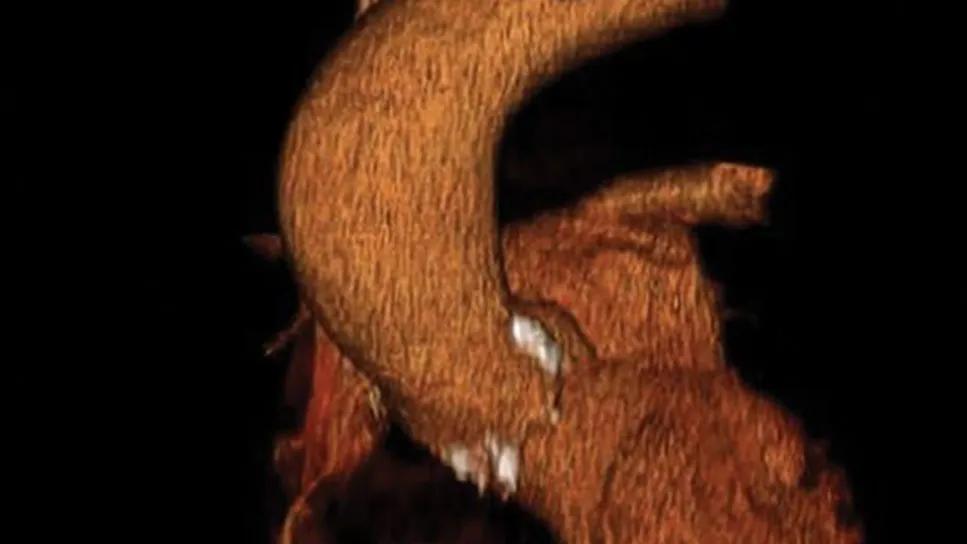
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/21d636d4-6367-401f-8e96-8082fabf88f4/ascending-aorta-aneurysm)
image showing a bulge in the ascending aorta of the heart
Among patients with ascending aortopathy (AA), women experience significantly poorer long-term survival than men, even when they undergo surgical repair at higher rates and present with fewer cardiovascular comorbidities. So concludes new observational research from Cleveland Clinic’s Aorta Center published in the Journal of the American Heart Association (2025;14:e045827). The findings suggest current surgical thresholds inadequately protect female patients and underscore the need for sex-specific approaches to aortic intervention.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Most catastrophic aortic events among unoperated patients in the study occurred in women with aortic diameters below conventional size criteria for prophylactic repair. “This pattern raises pressing questions about whether existing guidelines leave female patients vulnerable during a critical window when intervention could be lifesaving,” says senior and corresponding author Milind Desai, MD, MBA, Medical Director of the Aorta Center.
“This analysis supports integrating sex-specific and height-indexed criteria into surveillance and intervention pathways for ascending aortopathy in order to improve patient selection for prophylactic surgery,” adds coinvestigator Lars Svensson, MD, PhD, a cardiothoracic surgeon and Chief of Cleveland Clinic’s Heart, Vascular and Thoracic Institute.
Although AA is often asymptomatic, it carries a serious risk of aortic dissection, rupture and death. While prophylactic aortic replacement is recommended upon reaching a surgical threshold, guidelines have evolved inconsistently due to limited definitive clinical trial evidence and an incomplete understanding of the natural history of AA.
Notably, data from the International Registry of Acute Aortic Dissection have shown that a sizeable number of dissections occur when the aortic diameter is below 5.0 cm, which argues against sole reliance on absolute diameter. This has led to increased emphasis on improving risk stratification, especially for women and those with borderline aortic sizes, by incorporating height-indexed measurements like the aortic height index (AHI) and the cross-sectional area to height index (CSAH). Although these metrics have been validated in various smaller samples with AA, their use is limited.
Advertisement
The current study builds on previous observations that women, despite potentially lower AA prevalence, may experience poorer prognosis, faster aortic growth and increased risk of complications and death even at relatively smaller aneurysm sizes. Despite these observations, current clinical guidelines for AA largely lack sex-specific recommendations.
The researchers analyzed sex-stratified outcomes among 14,244 consecutive adults seen at Cleveland Clinic from 2010 to 2023 with unrepaired ascending aortic dilation measuring at least 4 cm on transthoracic echocardiography. Patients presenting with acute aortic dissection/rupture were excluded. Comprehensive clinical and echocardiographic data were collected, including AHI and CSAH. Aortic surgical procedures performed during follow-up were recorded, with surgical decision-making based on existing guidelines for diameter, concomitant conditions or rapid growth.
The primary outcome was all-cause mortality, with aortic dissection, intramural hematoma and rupture at least six months after initial echocardiography as secondary outcomes.
The cohort included 2,992 women (21.1%) and 11,252 men (78.9%). While women were older (63.6 vs. 62.3 years), they had significantly fewer traditional cardiovascular comorbidities such as hypertension, diabetes, coronary artery disease, atrial fibrillation and dyslipidemia.
Despite similar maximal absolute ascending aortic diameters between the sexes (P = .06), women exhibited significantly higher height-indexed measurements than men: AHI of 2.81 versus 2.59 cm/m and CSAH of 10.3 versus 9.5 cm²/m. These differences persisted across both echocardiographic and CT imaging modalities. Notably, a lower proportion of women had ascending aortic aneurysms defined as ≥ 5 cm (20.6% vs. 22.8%; P = .04).
Advertisement
Although women underwent aortic surgery at a higher rate (28.2% vs. 25.6%, P = .002) with a low in-hospital mortality rate of 0.9%, they experienced significantly higher long-term mortality (14.2% vs. 11.2%; log-rank P < .001) over mean follow-up of 6.2 years.
Female sex was independently associated with higher all-cause mortality (hazard ratio [HR] = 1.14; P < .001) despite cardiovascular surgery during follow-up being independently associated with improved survival (HR = 0.81; P < .001).
Regarding aortic events, 355 patients (2.5%) experienced late dissection/rupture, and rates were significantly higher in women (3.8% vs. 2.2%; P < .001).
Among patients who did not undergo surgical repair (n = 10,523), the distribution of adverse events was especially striking. More than three-quarters of all deaths and aortic catastrophes in women occurred when maximal aortic diameter remained below 5 cm at initial assessment. When applying height-indexed thresholds, over 90% of complications developed in women whose AHI fell below 3.21 cm/m.
Additionally, among unoperated patients with aortic dimensions exceeding recommended surgical thresholds (diameter ≥ 5 cm, AHI ≥ 3.21 cm/m or CSAH ≥ 10 cm²/m), women had higher rates of both death and aortic dissection or rupture compared with men.
These findings make a strong case for a more nuanced and sex-specific approach to AA management, the researchers contend.
“Current American and European guidelines, which recommend surgery when absolute ascending aortic diameter exceeds 5.5 cm, appear to inadequately capture risk, particularly in women and smaller individuals,” says Dr. Desai. “The heightened mortality and dissection rates we observed in women, even at smaller absolute diameters and with fewer comorbidities, are stark and are consistent with prior data. They call for a significant shift in clinical practice.”
Advertisement
The Cleveland Clinic researchers urge clinicians to prioritize routine use of height-indexed metrics like AHI and CSAH in AA surveillance and decision-making. They say a recognition that risk inflection points for adverse events may occur at lower indexed thresholds than previously established, especially in women, is crucial for identifying at-risk patients who can benefit from earlier intervention.
“Moving beyond a ‘one size fits all’ diameter-based approach allows for more precise risk assessment and, consequently, more timely and appropriate surgical intervention,” Dr. Svensson concludes. “This personalized strategy, particularly when executed at experienced aortic centers with low operative mortality, represents the future of care for ascending aortopathy.”
Advertisement
Advertisement
Study finds comparable midterm safety outcomes, suggesting anatomy and surgeon preference should drive choice
New review distills insights and best practices from a high-volume center
Blood test can identify patients who need more frequent monitoring or earlier surgery to prevent dissection or rupture
Recent Cleveland Clinic experience reveals hundreds of cases with anatomic constraints to FEVAR
Multicenter pivotal study may lead to first endovascular treatment for the ascending aorta
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation
Large cohort study finds significant effect in men and nonsmokers
Impacts include major emphases on multidisciplinary teams, shared decision-making