BITA grafts themselves are rarely to blame, and outcomes can be good
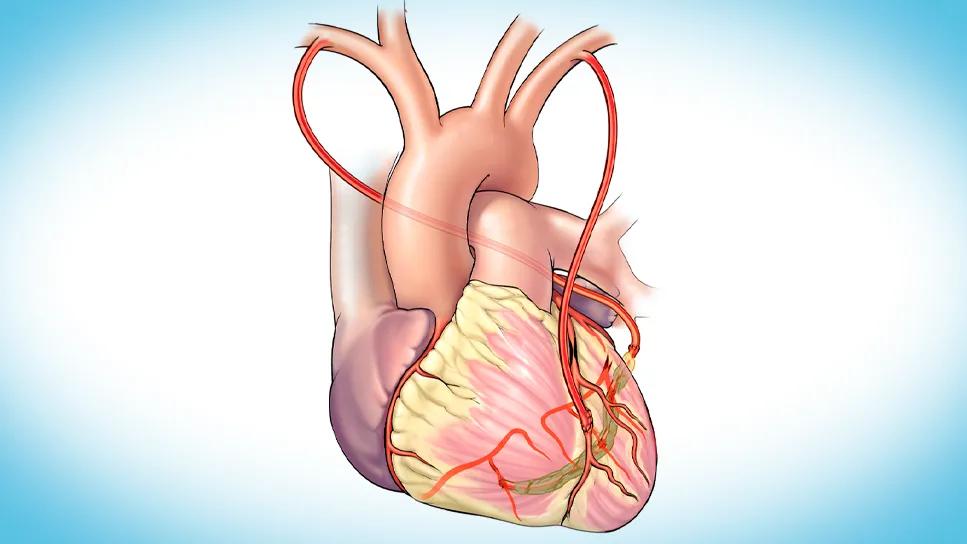
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b2c30f94-5492-4f2a-a489-ee26f589bf2e/CABG-grafts-CQD-feature)
human heart illustration showing coronary bypass grafts
Bilateral internal thoracic artery (BITA) grafts are widely regarded as offering superior protection against future cardiac reinterventions due to their excellent long-term patency and survival benefits. What happens, however, when a patient with patent BITA grafts redevelops ischemic symptoms?
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A recent retrospective analysis from Cleveland Clinic reveals that redo coronary artery bypass grafting (CABG) in this rare and complex patient population can be performed safely and with good short- and midterm outcomes at experienced centers.
“BITA grafts deliver what can be thought of as a lifetime warranty for almost all patients, but we found that exceptions do exist,” says Faisal Bakaeen, MD, Director of Cleveland Clinic’s Coronary Artery Bypass Surgery Center and senior author of the study, which was published online in The Journal of Thoracic and Cardiovascular Surgery. “The primary drivers of redo CABG in these patients are progressive native coronary atherosclerosis and failure of non-ITA grafts, rather than issues with the BITA grafts themselves, in most cases. This underscores the importance of aggressive medical management to slow disease progression and meticulous initial grafting strategies.”
Multiarterial grafting with BITAs is a cornerstone of modern coronary revascularization due to its long-term benefits. Current guidelines typically recommend percutaneous coronary intervention (PCI) over redo CABG for patients with a patent left ITA to the left anterior descending artery (LAD), given the inherent risks of reoperation. However, when ischemic symptoms endure despite optimal medical therapy and even PCI, a redo CABG may become necessary. Advances in imaging and surgical techniques have made these reoperations safer over time.
“Given the limited data on this small subset of patients needing redo CABG despite having patent BITAs, we reviewed our large experience base at Cleveland Clinic to better understand these cases in an effort to optimize their management and outcomes,” Dr. Bakaeen explains.
Advertisement
The study reviewed 8,108 patients who underwent isolated redo CABG at Cleveland Clinic between January 1980 and July 2020. Of these, only 91 patients (1.1%) had patent BITA grafts at the time of reoperation.
These 91 patients were predominantly male (89%) and had a mean age of 62 years at redo CABG. Reoperation took place a median of 10 years after initial CABG.
The researchers analyzed coronary angiograms to assess graft status, coronary anatomy and the importance of grafted vessels. Patient characteristics, operative details, and postoperative morbidity and mortality were collected from quality registries and medical records. Long-term all-cause mortality was estimated using the Kaplan-Meier method, with follow-up extending beyond 10 years for half of the cohort.
All patients presented with ischemic symptoms, most often unstable angina (71%). The cohort had a high prevalence of comorbidities, including hypertension (81%), dyslipidemia (92%) and diabetes (35%). More than half (53%) had prior PCI, indicating the aggressiveness of their underlying coronary disease. The LAD had previously been bypassed with an ITA in 86% of patients.
The anatomic drivers for reoperation were clear:
Advertisement
Intraoperatively, ITA injuries were rare (4.4%). “This dispels some concerns about re-entry complications in these patients,” Dr. Bakaeen observes. “It suggests that with advanced preoperative imaging, careful surgical planning and experienced teams, the risk of ITA injury can be minimized.”
Most patients (77%) underwent multivessel grafting at reoperation. Saphenous vein grafts were the most frequently used conduits (82%), with arterial grafts (primarily radial arteries) used in 51%. Interestingly, the LAD, a common target in primary CABG, was bypassed in less than half (40%) of patients during reoperation, with the left circumflex (64%) and right coronary (59%) arteries being more frequent targets.
Postoperative outcomes were encouraging:
At the end of their study report, the Cleveland Clinic authors outline several principles for managing patients with a history of BITA grafting who present with recurrent ischemic symptoms:
Advertisement
“We have demonstrated that redo CABG can be done safely, even with patent BITA grafts,” says staff cardiac surgeon Donna Kimmaliardjuk, MD. “This reinforces the philosophy that we follow here at Cleveland Clinic: If patients, especially younger patients, can receive BITA grafting, then they should get BITA grafts to the most important coronary targets, as these grafts have the best durability.”
“BITA grafting has become a cornerstone of the durable revascularization options we offer at Cleveland Clinic,” adds interventional cardiologist Laura Young, MD. “It is uncommon that these patients require redo CABG, but this study highlights our ability to safely perform redo CABG in these patients when no other revascularization options are available. It emphasizes the role of our multidisciplinary team in helping to decide the best revascularization plan for our complex coronary disease patients, whether it be stenting or redo open heart surgery.”
Advertisement
Advertisement
Two cardiac surgeons explain Cleveland Clinic’s philosophy of maximizing arterial graft use
Cleveland Clinic-pioneered repair technique restores a 61-year-old to energetic activity
Study indicates lower in-hospital mortality and better long-term survival
How Cleveland Clinic supported an alliance hospital to improve early extubation practices
Why and how we’re using robotic assistance for qualifying CABG candidates
Findings undercut perceptions of radial artery as second conduit of choice
TVT Registry analysis could expand indication to lower surgical risk levels
Cleveland Clinic series finds favorable long-term results with this high-risk operation