Minimally invasive staging technique improves accuracy, reduces complications
Approximately 80 to 85 percent of patients with endometrial cancer survive long-term. But what about the small percentage of patients who end up dying from metastatic disease? When endometrial cancer is diagnosed, using the most accurate staging and treatment strategies is key to delivering optimal patient outcomes — especially when managing aggressive forms of the disease.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Minimally invasive staging techniques are enabling Ob/Gyn specialists to provide higher quality care to endometrial cancer patients. In this article, Robert DeBernardo, MD, a gynecologic oncologist and Director of the Peritoneal Surface Malignancy Program, discusses how sentinel lymph node detection provides a higher rate of cancer detection while reducing the risk of long-term complications.
Q: How has endometrial cancer treatment changed over the past 10 years?
A: We used to treat endometrial cancer by performing an abdominal hysterectomy. Now, we’re primarily using robotic or laparoscopic hysterectomy — and achieving similar or better patient outcomes. Minimally invasive techniques are now the preferred standard of care for both treatment and staging.
Q: What controversy has developed over surgical staging?
A: At the time of surgery, we have the option of removing lymph nodes to check for metastases. For patients with high-risk cancer with a poor prognosis, removing lymph nodes provides valuable information that will impact the treatment plan and our ability to cure endometrial cancer.
Removing lymph nodes involves significant risk. In fact, about 10 to 20 percent of patients will experience some type of complication following lymphadenectomy. The most significant complication is lymphedema, which can lead to long-term mobility issues.
Q: What is the goal of assessing lymph node involvement?
A: Most patients with endometrial cancer have a low risk of lymph node involvement. So there are two key questions at play: How do we identify candidates for surgical staging? And how many lymph nodes should be removed? Because of the risk of complications, we have to be somewhat selective. For example, if there’s a 1 percent chance that your lymph node could be positive, it’s probably not reasonable to remove 20 or 30 lymph nodes. If you have a 30 to 40 percent chance of involvement, lymphadenectomy is an option well worth considering.
Advertisement
Q: How is sentinel lymph node detection used to stage endometrial cancer?
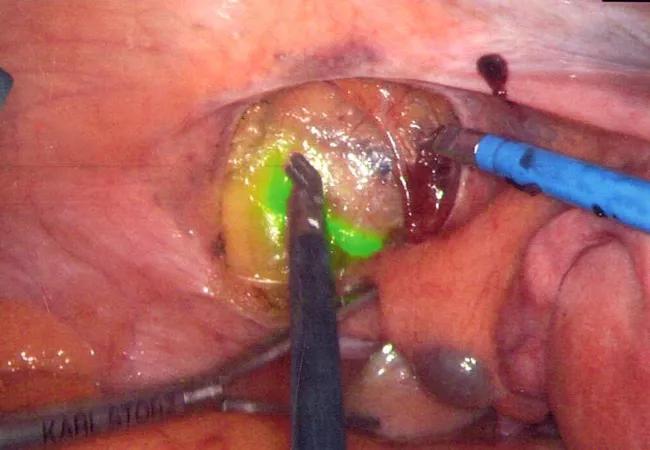
A: The sentinel lymph node technique has been used to identify lymph node metastasis in patients with melanoma, breast cancer and vulvar cancer. In patients with endometrial cancer, instead of injecting the tumor directly, we inject the cervix with the tracer dye. This technique still correlates well and reveals the activity of other lymph nodes. It also helps determine if radiation and chemotherapy should be used following a hysterectomy.
Q: How is the injection dye used?
A: We use an indocyanine green (ICG) dye that fluoresces so we can easily identify the lymphatic channels. This makes removing a sentinel lymph node very easy, avoiding complete lymph node dissection. By only removing the pertinent lymph nodes, we achieve a higher rate of metastatic cancer detection with fewer complications.
Q: Why is it important for Ob/Gyns to consider this staging technique before finalizing a patient’s treatment plan?
A: Sentinel lymph node detection can’t be used once a hysterectomy is performed. Patients at moderate or high risk will need a second surgery to remove all the lymph nodes or receive adjuvant radiation and/or chemotherapy to reduce the risk of recurrence. Patients being considered for endometrial cancer surgery should see a specialist with experience in sentinel lymph node detection.
Q: Are you aware of any research being conducted in support of this type of sentinel lymph node detection?
A: Future research will be used to assess the long-term cancer outcomes associated with sentinel lymph node detection in endometrial cancer patients. We expect them to be favorable.
Advertisement
To further advance cancer detection technology, we’re working on a bioengineering project that uses augmented reality to identify cancers and their resectability. The project is designed to capture computed tomography (CT or CAT) scans and magnetic resonance imaging (MRI) and create 3D images of patients. This will allow physicians to examine tumor location in relation to internal organs for more precise staging and treatment development.
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient