Study demonstrates superior visualization of occult primary lesions
Researchers at Cleveland Clinic recently demonstrated the accuracy of near-infrared fluorescence imaging in identifying small bowel carcinoid tumors and associated metastases intraoperatively. Infrared cameras were initially designed to visualize parathyroid disease, but the researchers found that many neuroendocrine tumors such as those in the adrenal gland, pancreas and small bowel show very distinct findings on fluorescence imaging. Their research showed that this new method is superior to conventional imaging, and is valuable for augmenting surgical inspection and palpation.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Carcinoid tumors of the small intestines are often less aggressive than other cancers, but they tend to be chronic. Between 40-55% of patients with this disease also have multiple lesions, some of which can be small and hard to find. For neuroendocrine and carcinoid tumors, removal of small bowel primaries is critical for improving survival, but current preoperative imaging is limited.
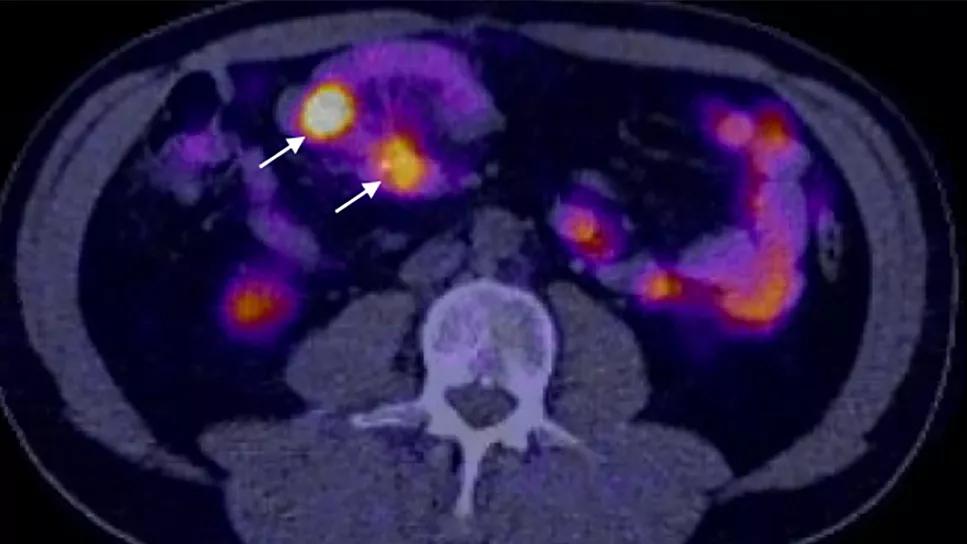
CT scans (7-38% sensitivity), CT enterography (76% sensitivity) and somatostatin receptor (16% sensitivity) approaches all fail to identify a significant number of lesions. Capsule endoscopy is another preoperative approach, yet its accuracy in identifying the number of tumors lies around 21%. This has left surgeons with inspection and palpation as the main preoperative method of identifying primary tumors.
Having treated many patients with this disease, Vice Chair of the Endocrine Surgery Center Eren Berber, MD, and his team began studying innovative diagnosis and treatment methods, such as near-infrared fluorescence. This new intraoperative imaging method involves using an infrared camera to detect fluorescence with indocyanine green injection.
On the heels of this discovery, a new method recently emerged that allowed surgeons to visualize tumors without the need for dye. The camera uses a harmless laser beam to identify tumors within seconds.
Dr. Berber’s team set out to compare this new method to existing imaging modalities such as DOTATATE PET scans. “When you look at these types of tumors through the infrared camera, it's almost like suddenly having night vision,” explains Dr. Berber. “They appear as bright dots.”
Advertisement
During small bowel resections with midline laparotomies for liver metastases, the researchers used a handheld camera to perform near-infrared fluorescence (NIRAF) imaging intraoperatively. Among all the carcinoids reported in pathology:
The data demonstrates a high degree of sensitivity of fluorescence imaging to detect small bowel primary cardioids. However, lesions that were deeply located beyond 1-2cm of the liver parenchyma could not be visualized, due to lack of deep penetration of the camera. The camera also does not appear effective in locating malignant mesenteric lymph modes or peritoneal metastatic foci.
“Our results show promise in the utilization of fluorescence imaging to detect occult primary tumors and superficial liver metastases,” says Dr. Berber. The findings suggest that routine incorporation of fluorescent imaging is beneficial for patients with small bowel carcinoid tumors. In addition to augmenting physician inspection and palpation, the camera may serve in guiding resections or ablations of superficial neuroendocrine liver lesions.
The Endocrine Surgery Center now routinely uses this technology during procedures. Incorporating this into the surgical technique helps the surgeon look closely at the small bowel to see if there is anything they’re missing through palpation. The team is continuing to evaluate the utility of this technique for intraoperative detection of thyroid, parathyroid, adrenal and pancreatic tumors.
Advertisement
Advertisement

Specialized care for a neonate with a rare condition

Navigating a complex case during a national copper shortage

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer