New device offers greater tumor control for malignant liver lesions

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1460739b-eb17-4a28-a073-7d6ad38eb76c/microwave-ablation-liver-cancer)
microwave ablation of liver tumor
150-watt microwave ablation has emerged as a non-invasive method for eradicating malignant liver tumors, as an alternative to traditional surgery in certain clinical scenarios, according to Cleveland Clinic’s Surgical Liver Tumor Ablation Program Director Eren Berber, MD.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Historically, surgical resection has been considered as the main option for treating malignant liver tumors, but this could be a major undertaking. Open surgery typically requires a five- to seven-day hospital stay and three to four weeks of recovery. Patients with systemic comorbidities may have a difficult time tolerating this extensive surgical procedure.
Although radiofrequency ablation was introduced as an alternative treatment modality for patients with unresectable tumors or who were otherwise not candidates for a liver resection, to date it has not been able to achieve the same level of disease control as liver resection. Microwave ablation has improved the treatment success, due to its ability to reach higher tissue temperatures more evenly to enable more effective tumor destruction.
Published data on liver ablation outcomes demonstrated that 100-watt microwave ablation systems reduced local treatment failures to less than 10% over radiofrequency ablation, which had failure rates of 20-40% for colorectal cancer metastases. However, these microwave ablations systems still had shortcomings, such as challenges with ablation of large and irregular tumors.
With FDA approval of a 150-watt microwave generator in 2020, Cleveland Clinic became the first center in the world to use the device to destroy a large liver tumor. Early results showed better cancer control rates. To date, Dr. Berber has performed the procedure on more than 200 patients. Using ultrasound guidance during the procedure makes it possible to obtain better visualization than other preoperative imaging techniques and discover additional lesions in 10-20% of patients.
Advertisement
Building on this work, Dr. Berber sought to evaluate patients on a larger scale to determine how they were faring after liver tumor ablation with the 150-watt microwave system.
The procedure is done through two 1-cm incisions in the right upper quadrant, with patients able to go home the next day. After the first global use of the technology in 2020, Dr. Berber and his team analyzed the early results by comparing the feasibility, safety and efficacy of liver ablations using the 150-watt microwave ablation system to those who underwent microwave ablation in the past with the 100-watt system. This initial study included a total of 33 patients with 76 malignant liver tumors treated with the 150-watt system, compared to 46 patients with 116 malignant liver tumors treated with the 100-watt system.
The data showed that the new, more powerful system made a notable difference in efficacy. “I was pleased to see that the ablations were faster with the 150-watt system, which meant shorter operations and less anesthesia time for the patients,” says Dr. Berber. “We were able to treat larger tumors in a shorter period of time without compromising treatment success compared to historical experience.”
The study demonstrated that use of the 150-watt device made it possible to treat tumors in a wide range of sizes in all segments of the liver in a safe and efficient manner. “There is a misconception that you can’t ablate a liver tumor that is on the surface of the liver or that is close to hepatic veins,” says Dr. Berber. “The laparoscopic approach makes it possible to destroy tumors in these difficult-to-access locations.”
Advertisement
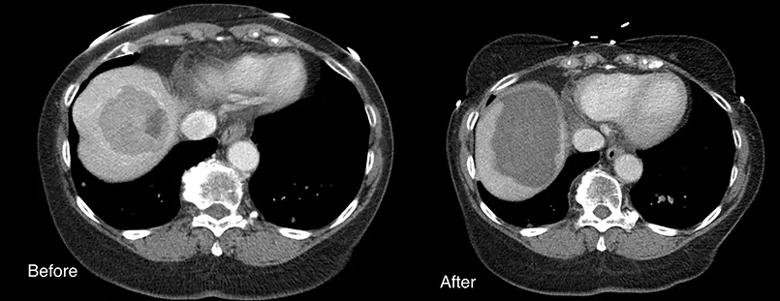
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/93cdbacd-32aa-4ce3-8f00-64e7d847124d/before-after-liver-tumor-ablation)
Using the more powerful system resulted in a low rate of complications (5%). Many ablation modalities require multiple liver punctures ‘sticks’ to be able to ablate a wide enough area to destroy cancer cells. This increases the risk of bleeding, as well as costs when multiple antennas are used. The study found an ablation zone of 6-7 cm could be created with the 150-watt device in 10 minutes, compared to a 4cm zone with the 100-watt device. This theoretically allows for larger margins and better tumor control.
Previous modalities had limitations in terms of the number of tumors that could be ablated in one session due to long operative times. The higher-powered device creates the necessary ablation cycles in a shorter amount of time compared to previous ablation system, allowing multiple lesions to be treated in a reasonably short time. These technological advances translate into significant patient benefits, such as minimally invasive treatment of small cancers deeply located in the liver with laparoscopic microwave ablation to allow for parenchymal preservation rather than removing a large amount of liver volume potentially with open surgery. Ultimately, this leads to a better quality of life and stronger immune system for the patient.
“There is a good deal of interest in emerging ablation technologies, as patients are seeking minimally invasive treatment options,” says Dr. Berber. “More data is needed to fully understand how much devices like this will improve local tumor control, particularly for larger tumors. Our evaluation is still ongoing. Nevertheless, I am pleased to offer patients more effective, minimally invasive treatment options for various types of liver cancer.”
Advertisement
Advertisement
Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence
Findings could help clinicians make more informed decisions about medication recommendations
Findings are first to provide underlying explanation, linking the diagnosis to high-immune activation and worse clinical outcomes
Histotripsy is noninvasive and may generate abscopal effect
IBAT inhibitors, elastography and more
Reviewing how the drug can be incorporated into care
Standardized and collaborative care improves liver transplantations
Cleveland Clinic specialists discuss challenges and opportunities for managing the disease