New and ongoing studies aim to reduce the need for surgery, improve risk stratification
Two current studies of patients with hypertrophic cardiomyopathy (HCM) serve as a sign that HCM management may be one of the fastest-maturing realms of contemporary cardiovascular care.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Our understanding of HCM has progressed to the point that we are developing novel medical treatments that will, hopefully, avoid the need for septal reduction therapy,” says Milind Desai, MD, Director of Cleveland Clinic’s Hypertrophic Cardiomyopathy Center.
One such medical therapy is the focus of one of the two above-mentioned HCM studies, both of which involve Dr. Desai among their lead investigators. The other is a National Institutes of Health-funded registry study that is using advanced imaging techniques to improve risk stratification in the disease. “That investigation represents an important first step in finding a way to reduce morbidity and mortality from HCM in a cost-effective manner,” notes Dr. Desai, who is also Director of Clinical Operations in Cleveland Clinic’s Department of Cardiovascular Medicine.
HCM is a chronic, progressive condition characterized by excessive contractions that cause heart muscle to thicken. In its obstructive form, the wall of the septum can become thick enough to obstruct outflow from the left ventricle to the aorta. As the outflow gradient rises, patients may experience debilitating symptoms that interfere with activities of daily living, and their risk increases for atrial fibrillation, stroke and heart failure.
The septal wall thickness can be reduced by septal reduction therapy, in the form of surgically removing excess tissue via septal myectomy or injecting alcohol into the heart muscle to ablate excess cells (alcohol septal ablation). Both approaches serve to relieve the obstruction and provide symptom relief, but neither form of septal reduction therapy addresses the underlying cause of HCM. And no effective noninvasive treatment options are now available.
Advertisement
Mavacamten is a novel oral medication being developed as an alternative to septal reduction therapy. It works to reduce muscle contractility by normalizing the number of myosin-actin cross-bridges that drive the excessive contractility, left ventricular hypertrophy and reduced compliance that characterize HCM.
“When the muscle does not contract so vigorously, obstruction is reduced, the gradient is lowered and patients feel better,” Dr. Desai explains. “As a result, they may not need surgery or ablation to manage their symptoms.”
Dr. Desai is serving as national principal investigator of the newest clinical study of mavacamten — a blinded, placebo-controlled trial to determine whether this agent can be an effective alternative to SRT.
The phase 3 trial, known as VALOR-HCM, will begin enrollment in the first half of 2020, with the goal of accruing 100 patients referred for septal reduction therapy at 15 leading HCM centers, including Cleveland Clinic. Patients will be randomized to mavacamten or placebo and then evaluated at 16 and 32 weeks to determine whether or not to proceed with septal reduction therapy.
One pressing question to be addressed is the long-term effect of reducing contractility. “We don’t know whether it will lower ejection fraction and cause heart failure, although that hasn’t been seen in preliminary studies,” notes Dr. Desai.
Findings from VALOR-HCM will supplement data from the ongoing phase 3 EXPLORER-HCM study of mavacamten in patients with symptomatic (NYHA class II or III) obstructive HCM. Top-line data from that trial are expected in the next few months. Long-term follow-up studies of patients treated with mavacamten are also ongoing.
Advertisement
If the trials are favorable, within the next two to three years mavacamten could become the first medical therapy approved for HCM. “If this agent can eliminate or reduce the need for surgery, it will be powerful,” says Dr. Desai.
VALOR-HCM is being run by the Cleveland Clinic Coordinating Center for Clinical Research (C5Research), with Steven Nissen, MD, Chief Academic Officer of Cleveland Clinic’s Miller Family Heart, Vascular & Thoracic Institute, chairing the study’s executive committee.
While a medical treatment clearly would be welcomed by patients with debilitating HCM symptoms, current methods of predicting these patients’ likelihood of developing heart failure or experiencing sudden cardiac death are limited. The Novel Markers of Prognosis in Hypertrophic Cardiomyopathy, or HCM Registry (HCMR), study was undertaken to identify which HCM patients are at increased risk for these catastrophic outcomes.
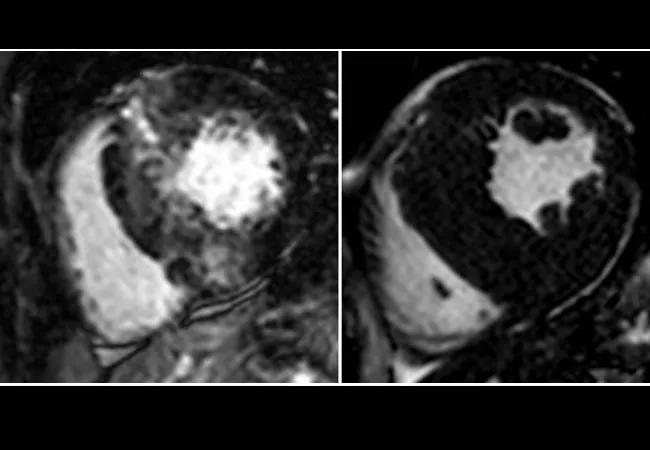
“Our aim is to develop a predictive model of cardiovascular outcomes in HCM by using exploratory data mining methods to identify outcome-associated variables, including demographic, clinical, genetic, biomarker and novel cardiovascular magnetic resonance [CMR] variables,” explains Dr. Desai, who serves on the study’s steering committee.
Cleveland Clinic is one of over 40 North American and European centers that have enrolled 2,755 patients in the observational study, the first large prospective registry of patients with HCM. All patients have undergone CMR imaging and other testing conducted under uniform protocols.
Advertisement
CMR is emerging as a powerful tool for diagnosis and risk stratification in HCM, including assessment of left ventricular mass and pattern of hypertrophy. Late gadolinium enhancement by CMR is a marker of focal myocardial fibrosis, which is thought to underlie the arrhythmogenic substrate and promote development of heart failure.
“We hypothesize that HCM patients with higher primary outcome event rates can be identified by novel CMR findings,” says Dr. Desai. “This could be helpful in developing therapeutic targets aimed at altering the phenotypic expression to impact the natural history of HCM.”
Baseline findings were published last November in the Journal of the American College of Cardiology(2019;74:2333-2345). Further results are expected this year and periodically as events occur over the study’s five-year follow-up period.
“Our goal is to develop novel tools that identify at-risk patients early in their disease course,” says Dr. Desai. “Once this study is completed, we believe it will change our ability to stratify risk.”
Image at top: CMR images representative of those from participants in the HCM Registry study.
Advertisement
Advertisement

Scenarios where experience-based management nuance can matter most

Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients