Lowers morbidity, improves quality of life
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
By age 80, 55% of women have more than two pelvic floor disorders as weakening of the pelvic floor and associated structures causes simultaneous prolapse of both the rectum and pelvic organs. In patients presenting with rectal prolapse, the concurrent rate of pelvic organ prolapse is 21% to 34%.
Traditionally, rectal prolapse (RP) and pelvic organ prolapse (POP) are corrected in separate surgeries. Combining these surgeries into one is not only appropriate, but eliminates the need for two anesthesias, hospitalizations and recovery times, and lowers the need for pain medications and time off from work and family duties. Repairing both problems at one time improves quality of life by reducing pain, bulge, constipation, urinary retention and bowel and bladder incontinence.
A number of different techniques are available to treat RP and POP. The optimal choice depends on the patient’s overall health, prior abdominal surgeries, presence of the uterus and feelings about mesh or biological graft.
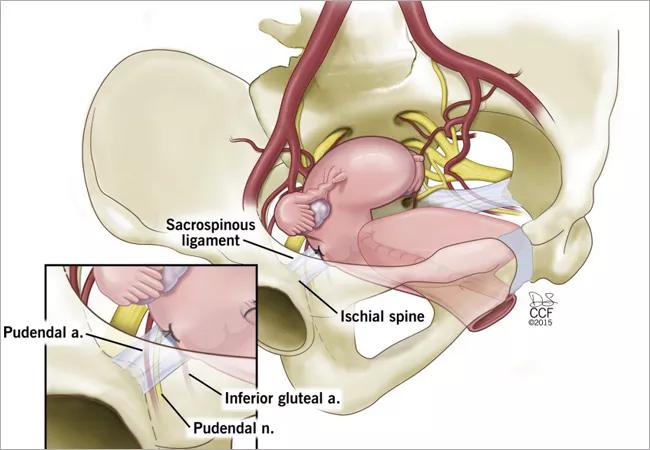
A perineal or transvaginal approach is recommended for frail patients, as well as those whose abdominal access may be compromised.
In younger and healthier patients, a laparoscopic or robotic abdominal approach is often preferred. The rectal and vaginal prolapse may be repaired by ventral rectopexy and sacrocolpopexy using a mesh or graft.
Recurrence rates for minimally invasive surgery for RP and POP are equivalent to those of open surgery. The advantages of minimally invasive surgery include shorter length of stay and faster return of bowel function. Patients have less pain and require less narcotics. They become mobile must faster and have fewer postoperative complications.
Advertisement
In a single-center study of 63 women who underwent surgical correction of combined RP and POP from 2008 to 2019, 18.3% experienced complications within 30 days. Most were minor: 82% were Clavien-Dindo grade 1 or 2. Rates of complications were similar between patients who underwent perineal procedures and those who underwent abdominal procedures. It is important to note that no complications occurred in patients who had undergone minimally invasive surgery, compared with 37.5% of the laparotomy group.
Overall, the need for RP repair for recurrent RP was 14%. The need for subsequent surgery for recurrent POP was 4.8%. There was no statistical difference for repeat RP surgery in patients who had undergone abdominal RP repair, compared with perineal RP repair. There was no statistical difference for repeat POP surgery in patients who had undergone transvaginal POP repair, compared with abdominal POP repair.
When we examined potential risk factors, age, body mass index, anesthesia risk score, history of smoking, prior RP and POP surgery, preoperative POP stage, hysterectomy at the time of surgery and surgical approach were not associated with either recurrence or complications after combined surgery.
On univariate analysis, the only significant risk factor for repeat RP surgery was colpocleisis at the time of transvaginal POP surgery. When adjusted for age—a known risk factor for both surgical complications and RP recurrence—colpocleisis was no longer a statistically significant risk factor for RP recurrence.
Advertisement
The only significant risk factor for complications from combined RP and POP surgery was laparotomy. When adjusted for age, laparotomy was no longer statistically significant, but approached significance.
A second prospective study was performed between 2017 and 2020 at the same institution. This study followed 70 patients with RP who underwent RP-only surgery and 45 patients with RP and POP who underwent combined RP and POP surgery. Although patients undergoing combined RP and POP surgery had a higher risk of complications, most of these complications were minor, including urinary retention and UTI. Both groups had equivalent recurrent RP rates similar to those rates seen in the previous study.
In our multidisciplinary pelvic health clinic, we screen patients with urinary complaints, symptomatic prolapse and defecatory dysfunction, and provide a combined consultation and evaluation. The ultimate benefit is a comprehensive, patient-centered approach and single, coordinated surgery. In our experience, combined procedures can be offered to patients with the advantages of a single operation and concurrent recovery period without increasing complications or inferior outcomes.
Advertisement
Advertisement

Multidisciplinary teams work together in in-situ scenarios

Uterine transposition cleared the field for radiation therapy

ACOG-informed guidance considers mothers and babies

Prolapse surgery need not automatically mean hysterectomy

Artesunate ointment shows promise as a non-surgical alternative

New guidelines update recommendations

Two blood tests improve risk in assessment after ovarian ultrasound

Recent research underscores association between BV and sexual activity