Recent research underscores association between BV and sexual activity
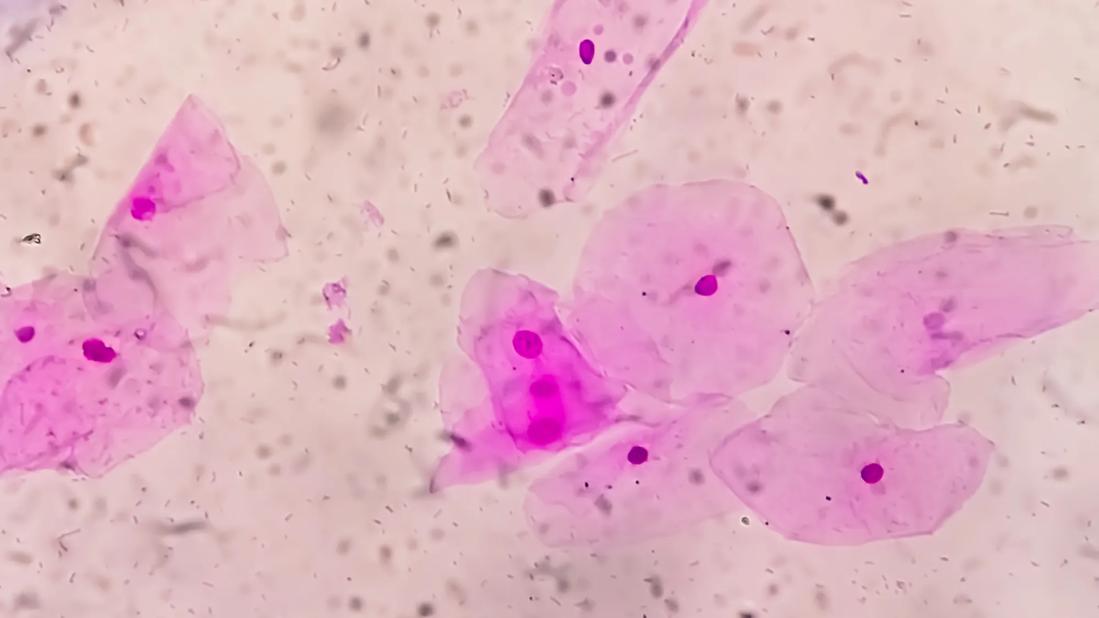
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5dde2368-7316-42aa-b4f0-178f3006be2c/bacterial-vaginosis-1456186941)
Slide image of bacterial vaginosis
Repeated bouts with bacterial vaginosis sometimes inspire patients to try all kinds of remedies with the hope of getting well. They may change their diet, clothing, and feminine hygiene products. They try over-the-counter supplements. These methods usually go along with the oral or topical antibiotics prescribed by their doctors, which, for this patient group, tend to work for a while before the infection returns.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Recurrences are frustrating, and over time the condition can have a significant effect on their quality of life and relationships.
Bacterial vaginosis (BV) is a common gynecologic condition — the one that most often sends women to their doctors. It’s a complex vaginal dysbiosis, and while it has long been recognized as having a connection to sexual activity, it also occurs in the absence of sex.
In March 2025, however, the New England Journal of Medicine published an Australia-based study showing that treating BV like a sexually transmitted infection (STI), and treating patients’ male partners with oral and topical medications, led to a lower rate of recurrence of BV.
Among results of the research were controversial headlines declaring BV an STI, as well as a suggestion that the time had come for changing treatment guidelines to include medicating patients’ partners.
At Cleveland Clinic’s Obstetrics and Gynecology Institute, Oluwatosin Goje, MD, Medical Director of the Center for Infant and Maternal Health, is focused less on the STI labeling and more on counseling patients to lean into practices proven to be helpful in reducing recurrences.
Dr. Goje’s own research on BV includes a comparison of the microbiome of patients with acute recurrent BV to healthy controls. She examined the effects of metronidazole on “good” and “bad” flora in participants with BV. Improvements in the balance were noted in the first week, but were not sustained. Meanwhile, the treatment arsenal for BV remains limited. CDC treatment guidelines have remained unchanged for years: metronidazole and clindamycin.
Advertisement
That makes the question of how those medications are used of significant interest to researchers hoping to find a breakthrough.
“The Australian study strengthens the hypothesis that BV is sexually associated, and that encouraging patients to change their diet or change their undergarments can be unnecessarily stressful,” says Dr. Goje. “They come back and mention that they have changed these things, and nothing is working. Those changes might be good for hygiene and for staying healthy, but we don't think they make a difference with BV.”
The research
The premise of the Australian study was that heterosexual sex partners share common microbiome. The researchers enrolled women who were in a monogamous, heterosexual relationship for at least eight weeks with a partner willing to use treatment. The women were all tested for BV and treated with oral antibiotics. Their partners were not tested for BV. Men in the intervention group received oral metronidazole and 2% clindamycin topical cream to apply to the penis. Men in the control group received nothing.
Among the 81 couples in the intervention group, there was a 35% infection-return rate. Infection returned for 63% the control group (81 couples). The study was stopped early because participants did significantly less well when the men were not treated. Forty-six percent of the treated men experience adverse events, including headache, nausea and a metallic taste.
The research, says Dr. Goje, suggests that treating male partners may be useful for some patients with BV. She adds, however, that “if BV is sexually associated, patients who are sensitive to changes in their bacterial flora might benefit if their partners use condoms. This is easier than getting medication into the hands of everybody involved, especially for patients who have multiple partners or who serially change partners. This is in addition to medication suggested by a provider.”
Recurrent versus refractory BV
Dr. Goje notes that there is a difference between recurrent and refractory BV. Testing reveals that for some patients, BV goes away with treatment and then comes back. BV is characterized as recurrent when the person has three episodes within one 12-month period.
Advertisement
For patients with refractory BV, treatment fails to relieve symptoms.
“For them, we have been adding boric acid vaginally, which can disrupt a biofilm that can cover the vagina and prevent adequate penetration of the medication,” she says. “So in patients with refractory BV, it's possible that it's due to that biofilm, and two medications — the boric acid vaginally and an oral medicine — can be more beneficial than just using the boric acid alone or the oral medicine alone.”
One study (Reichman et al, 2009) showed that adding vaginal disruptors are helpful, she says, “but when you think about the pathogenesis of BV, even though it's complex and we don't have the full picture, I think it's helpful if you're able to break the biofilm in an infectious process.”
Advertisement
Advertisement
Treatment being offered in cases where medical and hormonal management was not successful
Education, lifestyle modifications and new drug therapies can help
Multidisciplinary teams work together in in-situ scenarios
Uterine transposition cleared the field for radiation therapy
ACOG-informed guidance considers mothers and babies
Prolapse surgery need not automatically mean hysterectomy
Artesunate ointment shows promise as a non-surgical alternative
New guidelines update recommendations