Phase 2 clinical study supports safety and efficacy of MSC-NTFs
A phase 2 multisite study involving intrathecal injections of autologous mesenchymal stem cells (MSCs) enhanced to secrete neurotrophic factors (NTFs) demonstrated safety and preliminary evidence of efficacy in patients with either primary or secondary progressive multiple sclerosis (MS). Study findings were presented by principal investigator Jeffrey Cohen, MD, at the 2021 digital congress of ECTRIMS (European Committee for Treatment and Research in Multiple Sclerosis).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“It’s encouraging to see these outcomes for progressive MS, which has few good treatment options,” says Dr. Cohen, Director of the Experimental Therapeutics Program at Cleveland Clinic’s Mellen Center for Multiple Sclerosis Treatment and Research, one of the study sites. “We have learned more effective ways of preparing and delivering stem cells, with promising results.”
While more than 20 disease-modifying medications are available for treating MS, they are primarily helpful for relapsing-remitting disease, which has a strong inflammatory component that can be targeted with anti-inflammatory therapy. In contrast, people with progressive MS have already experienced inflammatory destruction, so they need therapy that can also repair damage.
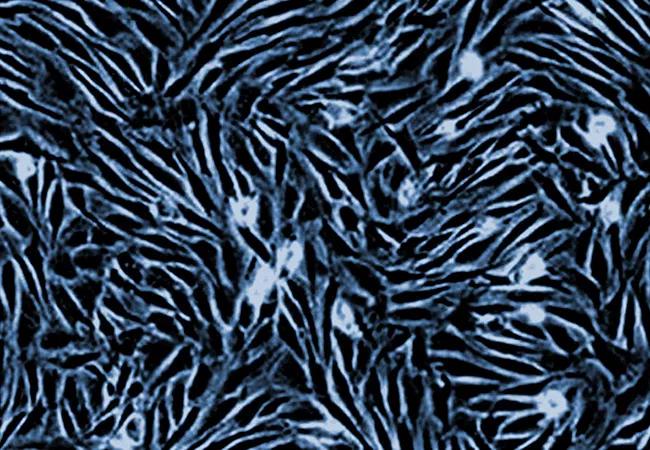
Autologous bone marrow-derived MSCs offer a potential treatment for progressive disease, but while earlier trials have demonstrated safety, they have shown only modest efficacy. Evidence indicates that modifying the stem cells in culture after harvest to secrete high levels of NTFs, microRNA and cytokines may enhance neuroprotection and immunomodulation. In addition, delivery directly into the cerebrospinal fluid appears more effective than intravenous injection, and multiple injections are likely needed to improve clinical benefit. These features were incorporated into the current trial.
The study took place between March 2019 and March 2021, enrolling 20 participants with either primary or secondary progressive MS at four U.S. sites. All had moderate to severe disability (mean baseline Expanded Disability Status Scale score of 5.4 — i.e., ambulatory without assistance, but disability impairs daily activity). Mean age was 47 years; 56% were female.
Advertisement
Bone marrow aspiration was conducted at the local sites, with aspirates sent to a central facility for in vitro cell culture and differentiation. After shipment back to local sites, 100 to 125 M MSC-NTF cells were injected intrathecally at weeks 0, 8 and 16.
Two participants were withdrawn because cells from their bone marrow aspirate failed to grow adequately. Of the 18 participants treated, 16 received all treatments and completed the study, including follow-up at week 28. Two participants withdrew, one due to procedure-related arachnoiditis.
To assess efficacy, these patients were matched to 46 control participants in CLIMB (Comprehensive Longitudinal Investigation of Multiple Sclerosis at Brigham and Women’s Hospital), a long-term observational study of patients with MS.
The primary endpoint was safety. Headache and back pain from the lumbar punctures were the most common side effects reported. There were no deaths and no treatment-related adverse events due to worsening MS.
Measures of efficacy and results in treated participants were as follows:
Advertisement
For the timed walking speed and peg tests, none or substantially fewer of the matched controls achieved these improvements — in fact, controls worsened slightly on many of the measures during comparable follow-up.
Additionally, cerebrospinal fluid biomarkers obtained from treated participants across three consecutive time points showed the following improvements:
“Everything went in the right direction,” says Dr. Cohen. “Because the study was small and did not include a control group, we must interpret the results with caution, but they are very encouraging.”
He notes that one purpose of the study was to work out the technical details and practical aspects of cell production, shipping and intrathecal administration. Lessons learned will assist in planning future studies, he adds.
“This study represents an important step in developing a much-needed effective treatment for progressive MS,” he concludes.
The study was funded by Brainstorm Cell Therapeutics.
Advertisement
Advertisement

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does

Novel Cleveland Clinic project is fueled by a $1 million NIH grant