Improving access to lifesaving kidney transplant

Approximately 90,000 patients in the United States are registered for a kidney transplant, according to data from the United Network for Organ Sharing (UNOS). The shortage of kidneys—and other lifesaving organs for transplantation—has led to urgent calls for improved organ utilization efforts worldwide.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Experts from Cleveland Clinic’s Kidney Transplant and Infectious Disease Programs continue to put forth protocols that guide transplantation for kidneys that may have been otherwise ineligible.
With limited guidance about best practices, transplanting extrapulmonary organs from deceased donors infected with SARS-CoV-2 has been controversial.
The Organ Procurement and Transplant Network (OPTN) Ad Hoc Disease Transmission Advisory Committee has emphasized balancing theoretical risk with potential waitlist-related complications or mortality. But with no other literature, transplant teams have had to take calculated risks.
In early 2021, the Kidney Transplant Team led by Alvin Wee, MD, MBA, Emilio Poggio, MD, and their infectious disease colleagues led by Christine Koval, MD, developed a protocol to perform kidney transplants from deceased donors who tested positive incidentally, without pulmonary issues. Continuing to monitor outcomes, they published their initial experience on 10 cases. Then they gradually expanded the criteria to include deceased donors with severe COVID-19 disease—as long as their kidney function was satisfactory.
Recently, the team published their experience of utilizing more than 100 kidneys from COVID-19-positive donors. In the American Journal of Transplantation, the authors report that from Feb. 1, 2021, to Jan. 31, 2022, they safely transplanted 115 adult kidneys from deceased donors with COVID-19. In total, 115 kidneys were transplanted from 68 donors with COVID-19, and 33 of these donors died from a COVID-19-related death.
Advertisement
Differences in graft performance and function were insignificant among the cohorts at a median follow-up of 5.7 months, regardless of SARS-CoV-2 status or severity. Recipients who received a kidney from a deceased donor with a COVID-19-related cause of death were associated with a lower—but still acceptable—estimated glomerular filtration rate at follow-up. Waiting time for an organ was shorter, the authors note.
Dr. Wee remarks: “Balancing the risk of accepting an organ with dying on the waitlist is always part of the decision when it comes to transplant, and the pandemic further complicated this. But this approach has enabled the transplant of more than 200 kidneys, a lifesaving intervention that may have been discounted otherwise. At the same time, this has also brought some meaning to the donor’s family from this senseless death.”
In September 2022, Cleveland Clinic performed a kidney transplant from a deceased donor with HIV to a patient with end-stage kidney disease who is HIV positive.
The legislation is part of a national effort to make transplantation more accessible to patients with HIV, reversing a decades-long policy that prevented people with HIV from donating organs, explains Anita Modi, MD, Associate Staff in the Department of Infectious Disease.
Dr. Wee, who performed the surgery, says now that the regulatory groundwork has been established, they are eager to offer this option to candidates who are HIV-positive to improve their access to a lifesaving and life-changing procedure.
Advertisement
Advertisement
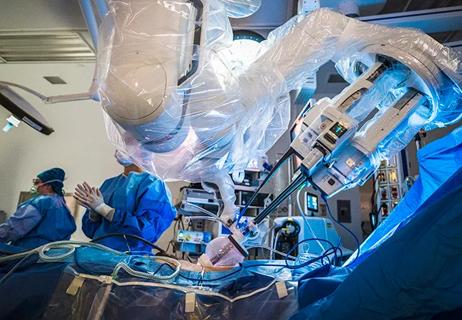
Surgeons choreograph nearly simultaneous procedures, sharing one robot between two patients

Smaller incision may lead to reduced postoperative pain for some patients
Key findings and proposed clinical interventions for affected areas

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more

Milestone minimally invasive surgeries reduce pain and recovery time

Veteran nurse blends compassion, cutting-edge transplant training and military tradition to elevate patient care

Enhanced visualization and dexterity enable safer, more precise procedures and lead to better patient outcomes

Insights on bringing Cleveland Clinic even closer to becoming the best transplant enterprise in the world