Newly identified pathway may explain the so-called niacin paradox

A Cleveland Clinic-led research team has identified a new pathway that contributes to cardiovascular disease independent of traditional risk factors. The pathway is linked to excess levels of niacin, a B vitamin common in the American diet and previously used to lower LDL cholesterol.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The team, led by Stanley Hazen, PhD, MD, discovered that a blood metabolite called 4PY, which results from excess niacin, is associated with increased incidence of major adverse cardiovascular events (MACE). They also found in mechanistic studies that 4PY directly leads to vascular inflammation and cardiovascular disease in preclinical models.
The group’s research, consisting of a series of investigations reported in a Nature Medicine article (Epub 19 Feb 2024), details the discovery of a link between 4PY and cardiovascular disease, genetic links between 4PY and vascular inflammation, and studies showing that 4PY promotes vascular inflammation. Such findings provide a foundation for potential new interventions and therapeutics to block this process.
“What’s exciting is that this pathway appears to be a previously unrecognized yet significant contributor to the development of cardiovascular disease,” says Dr. Hazen, Chair of Cardiovascular and Metabolic Sciences in Cleveland Clinic’s Lerner Research Institute and Co-Section Head of Preventive Cardiology in its Heart, Vascular & Thoracic Institute. “What’s more, we can measure it, meaning there is potential for diagnostic testing. These insights set the stage for developing new approaches to counteract the effects of this pathway.”
The findings also have potential implications for nutritional policy in the United States and beyond, the investigators note, in view of long-standing niacin fortification of grain-based food staples.
Advertisement
The research stems from ongoing efforts by Dr. Hazen and colleagues to identify new contributors to residual cardiovascular risk. The team follows patients over time and collects blood samples to find chemical signatures that can predict the development of cardiovascular disease. “Residual cardiovascular risk remains high in some patients despite guideline-directed therapy,” Dr. Hazen notes, “suggesting additional contributors beyond established risk factors for cardiovascular disease.”
For the current research, his team used an untargeted mass spectrometry platform to analyze fasting plasma from 1,162 patients with stable cardiac disease to screen for circulating small molecules that might be predictive of incident MACE independent of traditional risk factors. This analysis suggested a link between niacin metabolism and incident MACE.
The researchers subsequently found that plasma levels of two terminal metabolites of excess niacin — N1-methyl-2-pyridone-5-carboxamide (2PY) and N1-methyle-4-pyridone-3-carboxamide (4PY) — were significantly associated with elevated three-year MACE risk in U.S. (N = 2,331) and European (N = 832) validation cohorts.
After performing genome-wide association studies to identify genetic variants associated with 2PY and 4PY levels, they next conducted phenome-wide association analysis of a strong genetic variant identified, known as rs10496731. The analysis found this variant to be associated with levels of soluble vascular adhesion molecule-1 (sVCAM-1), a biomarker of endothelium dysfunction. This association was confirmed in a meta-analysis the researchers performed using their U.S. validation cohort combined with the U.K. Biobank and publicly available data from other cohorts, yielding a sample of 106,000 subjects. Further analysis corroborated sVCAM-1 levels to be significantly correlated with 2PY and 4PY in an independent 974-patient validation cohort from Cleveland Clinic.
Advertisement
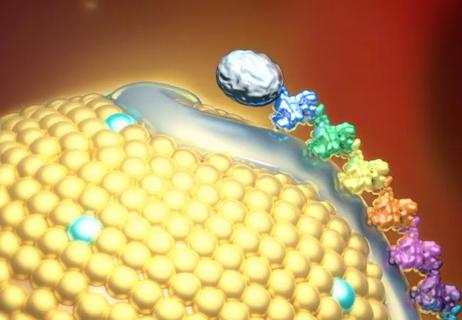
The researchers then conducted a series of functional studies to determine whether physiological levels of 2PY and 4PY fostered VCAM-1 expression in vitro on endothelial cells and in vivo in mouse aortic tissue. They found that treatment with physiological levels of 4PY, but not 2PY, promoted expression of VCAM-1 in vitro and in vivo, as well as leukocyte adherence to vascular endothelium, the primary function of VCAM-1, in mice using intravital microscopy.
“Taken together, these results demonstrate that these breakdown products of excess niacin — namely, 2PY and 4PY — are associated with residual cardiovascular risk,” Dr. Hazen observes. “They additionally suggest that an inflammation-dependent mechanism underlies the association of 4PY with major adverse cardiovascular events.”
The researchers note that their findings offer a compelling potential explanation for the so-called niacin paradox stemming from past use of niacin as a therapeutic agent to treat dyslipidemia. The paradox arose from clinical trial findings that while niacin reduces LDL cholesterol, it does not reduce risk of cardiovascular disease and has even shown evidence of increasing overall mortality.
“Despite niacin’s cholesterol-lowering effect, the clinical benefits have always been less than anticipated based on the degree of LDL reduction,” Dr. Hazen notes. “This led to the idea that excess niacin caused unclear adverse effects that partially counteracted the benefits of LDL lowering. We believe our findings help explain this paradox. This illustrates why investigating residual cardiovascular risk is so critical — we learn much more than what we set out to find.”
Advertisement
“This is an intriguing study and raises many questions,” adds Leslie Cho, MD, Co-Section Head of Preventive Cardiology at Cleveland Clinic, who wasn’t involved in the research. “More studies are needed to confirm this finding.”
The study authors note that long-term investigations are needed to assess the effect of chronic elevation of 4PY levels on atherosclerosis and other phenotypes. In the meantime, they write, their findings argue for discussion of whether current nutritional policy around niacin fortification should be revisited, especially for vulnerable populations.
“For decades, the United States and more than 50 other nations have mandated niacin fortification in staple foods such as flour, cereals and oats to prevent pellagra and other niacin deficiency syndromes,” Dr. Hazen explains. While this has successfully reduced pellagra deaths to a dramatic degree, he notes, there is now wide availability of foods naturally rich in niacin, and average dietary intake of niacin has increased to levels far exceeding recommended ranges. He wonders whether flour and cereal fortification, despite its remarkable success in preventing nutritional deficiencies since World War II, might have had the unintended consequence of contributing to the overall rise in cardiovascular disease over the past 75 years.
“In our studies, the highest quartile of 4PY levels was associated with an approximately twofold increased incidence of major adverse cardiovascular events compared with levels in the lowest quartile,” Dr. Hazen says. “One in four people in our cohorts had high levels of 4PY and are at significantly higher risk for adverse cardiovascular events.” In light of this, he and his co-authors contend, it might be reasonable to ease niacin fortification mandates to allow for nonfortified flour and cereal options to be available.
Advertisement
“The takeaway is not that we should cut out our entire intake of niacin — that’s not a realistic or a healthy approach,” Dr. Hazen says. He adds, however, that new scrutiny is needed of the widespread use of dietary supplements containing niacin, which are often taken for unsupported anti-aging effects. “Patients should consult with their doctors before taking over-the-counter supplements and focus on a diet rich in fruit and vegetables while avoiding excess carbohydrates,” Dr. Hazen concludes.
Advertisement

Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics

First-in-human phase 1 trial induced loss of function in gene that codes for ANGPTL3

Cleveland Clinic pioneers a new paradigm in cardiovascular care delivery

Site visits offer firsthand lessons in clinical and operational excellence in cardiovascular care

Phase 3 TANDEM study may help pave way to first approval of a CETP inhibitor

Yet 21.4% of tested individuals had Lp(a) elevation

AHA recommendations for pretransplant evaluation, peritransplant and long-term management
Phase 2 trial of zerlasiran yields first demonstration of longer effect with each dose of an siRNA