L. monocytogenes endophthalmitis is often difficult to diagnose and requires high clinical suspicion

By Careen Y. Lowder, MD, PhD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Listeria monocytogenes rarely affects the eye, but when it does, the outcome has often been poor, with reported final vision worse than 20/200. Listeria is a gram-positive bacteria that is transmitted through contaminated food. It can grow at refrigerator temperatures and may cross-contaminate foods that are prepared or stored in the same area. In 2016, there were 196 recalls of unpasteurized dairy products, meats, seafood, nuts, fruit, and raw and frozen vegetables due to Listeria contamination nationwide. Symptoms include fever and muscle aches, sometimes preceded by gastrointestinal symptoms. Unfortunately, the link to the consumption of contaminated food often goes unnoticed, as symptoms can appear days to weeks later.
L. monocytogenes endophthalmitis typically presents with eye pain, elevated intraocular pressure (IOP) and a fibrinous anterior chamber reaction. We present a case of endogenous L. monocytogenes endophthalmitis in a healthy man who recovered 20/20 vision after aggressive treatment with local and systemic antibiotics and anterior chamber washout.
A 58-year-old man was seen in Cleveland Clinic’s Emergency Department after two days of progressive right eye redness and pain. Vision was 20/400 OD and 20/20 OS. Intraocular pressure (IOP) was 51 mm Hg OD and 17 mm Hg OS. Slit-lamp examination of the right eye revealed 3+ conjunctival injection, corneal edema and fibrin on the endothelium. The anterior chamber was deep with a fibrinous reaction. His left eye was normal. The patient did not respond to maximum medical IOP therapy. An anterior chamber paracentesis was performed because he was symptomatic with nausea and headache. Despite medications, IOP was 43 mm Hg the next day in the glaucoma clinic. Vision improved to 20/70, and exam was unchanged. The patient was started on valacyclovir 1 gram three times a day and topical prednisolone acetate for presumed herpetic keratouveitis and referred to the uveitis service.
Advertisement
The next day, the patient’s vision dropped to 20/300, and IOP was 54 mm Hg. The patient was noted to have a 4 mm hypopyon (Figure 1). B-scan ultrasound showed anterior vitritis. An anterior chamber tap was performed, and intravitreal vancomycin and ceftazidime were injected for suspected infectious endophthalmitis. The patient was started on hourly fortified vancomycin and ceftazidime drops. On the following day, the patient’s vision dropped to hand motion, and the hypopyon was larger. Prednisone 80 mg daily was started, and the hypopyon was even larger the next day (Figure 2). At this time, the anterior chamber tap grew L. monocytogenes.
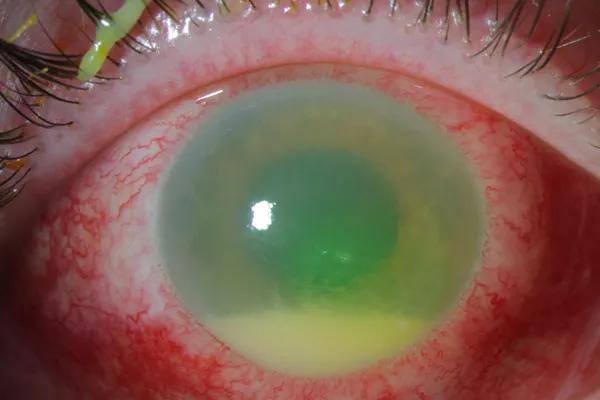
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/abb23ec7-ddf9-4cc5-b3be-055dbc7bfeb1/17-EYE-1416-Lowder-CQD-Inset-1_jpg)
Figure 1. A 4 mm hypopyon was noted two days after anterior chamber paracentesis, and IOP-lowering medications were initiated in a patient with Listeria monocytogenes endophthalmitis.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4f04a65c-b960-4a94-8b8e-daffdab4feb2/17-EYE-1416-Lowder-CQD-Inset-2_jpg)
Figure 2. Another day later, the hypopyon was even larger, and the patient’s vision had dropped to hand motion only.
The patient was immediately seen by an infectious disease specialist and started on a 30-day course of intravenous 3 gram ampicillin every six hours via a peripherally inserted central catheter. After our infectious disease consultant advised us of L. monocytogenes’ known resistance to vancomycin and ceftazidime, intravitreal amikacin was given and fortified antibiotic drops were changed to gentamicin for better coverage. Prednisone was discontinued. Due to persistent hypopyon, two oral double-strength trimethoprim-sulfamethoxazole tablets twice a day were added five days later. Prednisone was restarted at 60 mg daily and tapered over one month.
Advertisement
The patient’s vision and exam began to improve. His IOP remained controlled. However, his hypopyon consolidated into a dense mass that did not resolve (Figure 3), and he underwent an anterior chamber washout two weeks after initial presentation. His ocular antihypertensives and steroids were slowly tapered. Four weeks after anterior chamber washout, his vision was 20/20-1, IOP was 14 mm Hg off glaucoma medications and his eye was quiet (Figure 4).
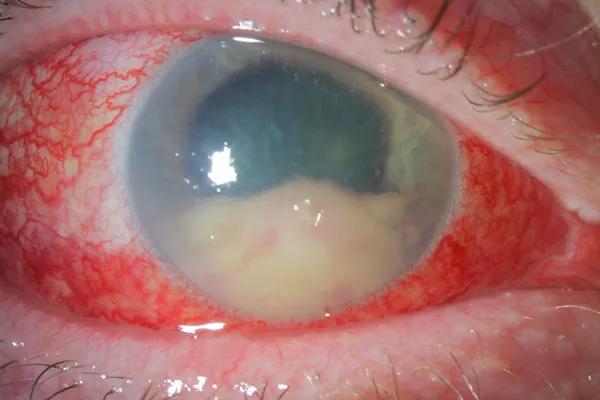
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9f2a4c52-744f-428a-b286-674ed42b0fd6/17-EYE-1416-Lowder-CQD-Inset-3_jpg)
Figure 3. Two weeks after initial presentation, the hypopyon consolidated into a dense mass, and the patient underwent an anterior chamber washout.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/691808ed-5f3e-47ba-8a23-dd7905237529/17-EYE-1416-Lowder-CQD-Inset-4_jpg)
Figure 4. Four weeks after the anterior chamber washout, the eye was quiet, and vision returned to nearly 20/20.
L. monocytogenes endophthalmitis is often difficult to diagnose and requires high clinical suspicion. Delayed diagnosis can allow significant inflammatory response to mount prior to appropriate antibiotic therapy. In the setting of a hypopyon with high IOP, Listeria should be considered and appropriate antibiotics administered, especially in light of increasing reports of Listeria food contamination. Given that Listeria endophthalmitis is most commonly endogenous, systemic antibiotics are an important complement to intravitreal antibiotics. At our institution, bacterial endophthalmitis is empirically treated with intravitreal vancomycin and ceftazidime. However, L. monocytogenes resistance to both of these agents is common.
Our case highlights the importance of early diagnosis and treatment, including proper laboratory evaluation, surgical intervention and interdisciplinary collaboration, for the best patient outcome.
Advertisement
Advertisement

Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma

Registry data highlight visual gains in patients with legal blindness

Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence

A look at emerging technology shaping retina surgery

A primer on MIGS methods and devices

7 keys to success for comprehensive ophthalmologists

Study is first to show reduction in autoimmune disease with the common diabetes and obesity drugs

Treatment options range from tetracycline injections to fat repositioning and cheek lift