Volume-based experience and judicious patient selection are central to success
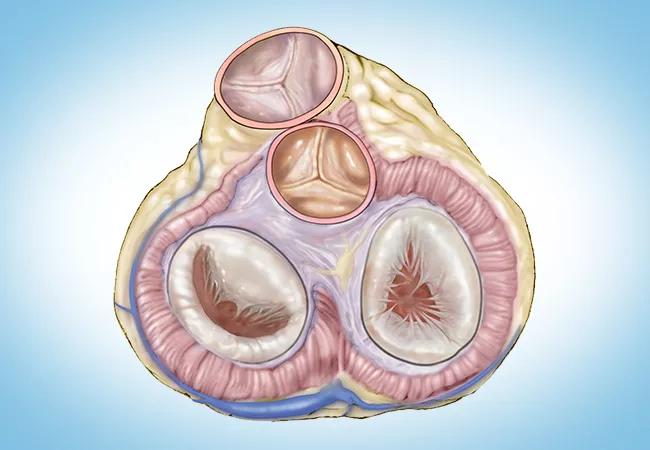
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/81f0d6c2-d790-422d-9b8c-a774d95d911b/23-HVI-4475649-CQD-650x450-1_jpg)
23-HVI-4475649 CQD 650×450
Elective reoperation involving multiple cardiac valves can be performed safely with low associated mortality, finds a Cleveland Clinic study of more than 2,300 patients who underwent reoperations involving repair or replacement of two or more valves. The study, one of the largest series of such cases ever published, reveals that the number of surgical components and the patient’s health status were important factors predicting operative risk.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Multivalve cardiac reoperation can be done successfully in high-volume centers with experienced surgeons and well-coordinated teams that optimize the patient’s condition preoperatively through recovery,” says Cleveland Clinic cardiothoracic surgeon Faisal Bakaeen, MD, corresponding author of the study published in the Journal of Thoracic and Cardiovascular Surgery (Epub 2023 Dec 9). “However, because the complexity and number of component procedures impact the risk of the operation, surgical judgment is crucial in determining which problems should be addressed.”
As valvular surgeries have advanced over the past decades and patients are surviving longer, many are more frequently presenting for reoperations with complex cardiac problems along with comorbidities of old age. While published data and risk models are available for single-valve reoperations, much less is known about the multivalve reoperative setting.
“With multiple patient and operative factors, a large database is needed to tackle this problem,” Dr. Bakaeen notes. In this series, Cleveland Clinic characterized its experience with multivalve reoperations over 14 years, with particular focus on intraoperative complications, outcomes and risk factors related to patient characteristics and surgery type.
A previous Cleveland Clinic study reported on outcomes from more than 6,500 cardiac reoperations, consisting mainly of aortic valve replacement, coronary artery bypass grafting (CABG), and aortic root and arch procedures (J Thorac Cardiovasc Surg. 2022;164[6]:1755-17666e16).
Advertisement
The cohort for the current study consisted of 2,342 adults who underwent 2,352 reoperations on multiple cardiac valves at Cleveland Clinic from 2008 to 2022. Nearly half of the operations were on women; average patient age was 66 ± 14 years. Other than valve disease, the most common cardiac comorbidities were coronary artery disease, heart failure and atrial fibrillation; other common problems were hypertension, chronic obstructive pulmonary disease, cerebrovascular disease and diabetes.
More than half of surgeries were elective (56%, n = 1,327), 43% were urgent (n = 1,006) and less than 1% were emergency (n = 19). First-time reoperations made up 76% of cases, with the remaining patients having had two or more prior operations. The median time since last cardiac surgery was 9.5 years.
Reoperation involved two valves in 80% of cases — most commonly mitral valve replacement plus tricuspid valve repair, followed by aortic valve replacement plus mitral valve replacement. Approximately 20% of cases involved three valves, and two patients had surgery on four valves.
Nearly half of the surgeries involved other procedures in addition to the multivalve reoperations — specifically, ablation procedures for atrial fibrillation (n = 577) and CABG (n = 528).
The number of surgical components totaled two in 43% of patients, three in 43%, four in 13%, and five or more in 1%.
Across the overall cohort, there were 98 operative deaths (4.2%) and 93 hospital deaths (4.0%).
Mortality rates were substantially lower among the study’s 704 patients whose reoperations were elective and did not involve concomitant non-valve procedures, specifically:
Advertisement
The authors note that these outcomes — even those for the overall cohort — compare favorably to those of two large prior studies that reported in-hospital mortality of 7.2% for isolated reoperations on the aortic valve (Monaldi Arch Chest Dis. Epub 2023 Apr 19) and operative mortality of 11.1% for isolated reoperations on the mitral valve (Heart. 2018;104:652-656).
Operative mortality approximately doubled with each additional surgical component, ranging from 2.4% (24/1,009) in reoperations involving two components to 16.7% (5/30) for those with five components.
Additional factors associated with higher mortality were concomitant CABG, preoperative renal dysfunction, low left ventricular ejection fraction (< 45%), New York Heart Association class III or IV, urgent or emergency surgery, anemia (hematocrit < 37%) and peripheral artery disease.
Dr. Bakaeen emphasizes several factors that are critical to successful outcomes for these complex multivalve reoperative procedures:
Advertisement
Dr. Bakaeen notes that a limitation of this nonrandomized series is that patients who were managed conservatively without surgery were not included for comparison. He adds that Cleveland Clinic surgeons tend to avoid surgery in extremely frail or compromised patients, and the study demonstrates that in select patients, multivalve reoperations can have excellent outcomes.
“Good judgment is absolutely critical when planning such complex reoperations,” Dr. Bakaeen observes. “Since higher complexity is associated with greater mortality, it is essential to consider which parts of the proposed surgery can be left unaddressed without affecting the patient during their lifetime, as well as which lesions can be addressed at a later date by a transcatheter approach.”
The study authors conclude by noting that transcatheter and hybrid therapies may one day play an important role in these multivalve reoperations, offering the potential of increased safety. More research is needed to determine comparative outcomes for different valves and devices, they note.
Amar Krishnaswamy, MD, Section Head of Interventional Cardiology at Cleveland Clinic, also sees this potential. “Catheter-based treatment options have become increasingly available and demonstrate excellent safety and efficacy in anatomically and clinically appropriate patients,” he notes. “At Cleveland Clinic we have a large practice of transcatheter valve replacement and repair. Unfortunately, for patients with multiple valve problems requiring reoperation, multiple transcatheter valve treatment options are usually not feasible.”
Advertisement
“At Cleveland Clinic,” he continues, “all patients considered for a transcatheter treatment as an alternative to cardiac surgery are assessed by interventional cardiologists as well as cardiac surgeons — along with nurses, nurse practitioners and clinicians from other cardiology subspecialties — so we can provide our best recommendation after consideration of their case from numerous angles. Whether the final recommendation is for cardiac surgery or a transcatheter treatment, the outcomes reported in this study show that we consistently provide the best option for a given patient.”
“We are fortunate to have national databases that compare outcomes among various centers,” adds Lars Svensson, MD, PhD, Chief, Cleveland Clinic Heart, Vascular & Thoracic Institute. “These tell us, for example, that Cleveland Clinic’s annual mortality rate for isolated aortic valve replacement, which ranges from 0% to 0.6%, is half the rate predicted by the Society of Thoracic Surgeons for 2023, with similar outcomes for TAVR. However, for complex valve reoperations, there is no national standard since no one treats these patients in large enough numbers. In this context, the low mortality rate of 1.7% in this study sets the standard for what can be expected for multivalve reoperations, particularly since transcatheter options cannot readily be used for this population of patients.”
Advertisement
Intentional culture of safety extends outcome gains to both novice and late-career surgeons
BITA grafts themselves are rarely to blame, and outcomes can be good
TVT Registry analysis could expand indication to lower surgical risk levels
A scannable recap of our latest data in these clinical areas
A scannable graphic recap of our latest data
Cleveland Clinic series finds favorable long-term results with this high-risk operation
Surgeons credit good outcomes to experience with complex cases and team approach
TRISCEND II trial reports 1-year results