Cleveland Clinic series supports re-repair as a favored option regardless of failure timing
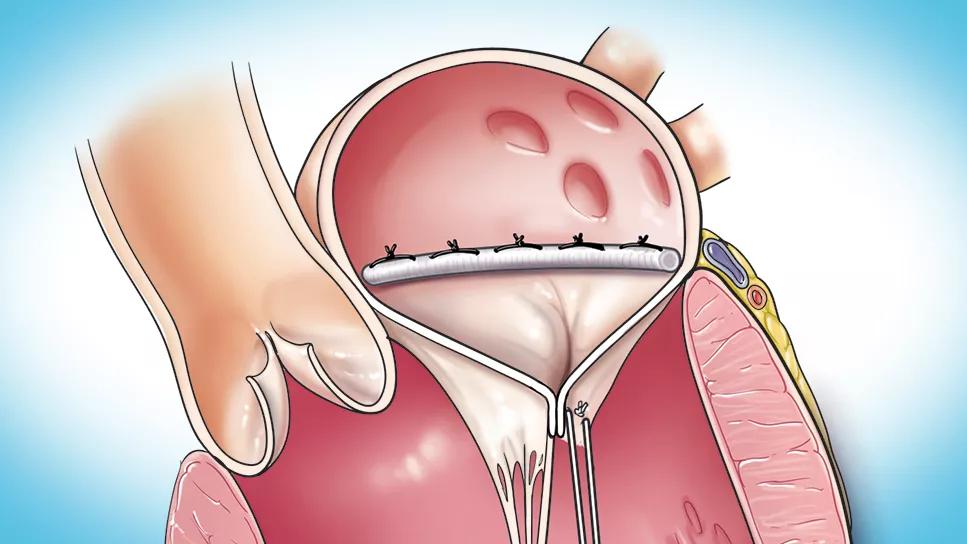
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9bab83b5-6572-4ad5-b861-875623103d42/completed-mitral-valve-repair-1)
completed mitral valve repair
In patients with degenerative mitral regurgitation (MR), mitral valve re-repair is associated with very low operative risk and a durable improvement in mitral valve function.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
So concludes a retrospective study of reoperation after early and late failure of mitral valve repair published in the Journal of Thoracic and Cardiovascular Surgery (2024;167[4]:1251-1262.e8). Although re-repair was most feasible when failure occurred early, the authors recommend it for late failures, too, as long as operative pathology allows.
“In our study, re-repair was associated with zero mortality, and at seven years after surgery, nearly all our patients were free from severe MR,” says senior author A. Marc Gillinov, MD, Chair of Thoracic and Cardiovascular Surgery at Cleveland Clinic. “In selected patients, mitral valve re-repair should be preferred to valve replacement whenever the procedure is technically feasible.”
When MR recurs after mitral valve repair for degenerative disease — which happens in fewer than 1.5% of patients annually, according to literature reports — the traditional approach has been mitral valve replacement. However, re-repair has become increasingly popular in the past 20 years as understanding of the mechanisms of valve failure has grown and repair techniques have improved. Recent studies have shown that re-repair can be safe, durable and associated with longer survival relative to replacement, especially when valve failure occurs within a year after a patient’s original surgery.
In the new study, Cleveland Clinic researchers explored factors that might contribute to early and late failure of initial mitral valve repair and identified factors associated with re-repair versus valve replacement.
Advertisement
Data analyzed were from 330 patients with a history of mitral valve repair for degenerative disease (i.e., mitral valve prolapse) who underwent reoperation at Cleveland Clinic for recurrent mitral valve dysfunction between January 2008 and July 2020. Among these patients (mean age, 63 years), 93 (28%) underwent re-repair and 237 (72%) underwent valve replacement.
In addition to analyzing the factors noted above, the study compared survival between patients undergoing re-repair versus replacement and tracked valve durability — assessed by longitudinal analysis of postoperative echocardiograms — and other clinical outcomes among those undergoing re-repair. Median duration of follow-up was 5.8 years, with 10% of patients followed for over 12 years.
The median time to reoperation was 3.1 years. Failure of initial mitral valve repair occurred early (i.e., within one year) in 85 patients (26%) and late (after one year) in 245 patients (74%).
Among those with early repair failure, the most common mechanisms of valve dysfunction were suture/annuloplasty dehiscence, systolic anterior motion, hemolysis and ventricular remodeling. Among those with late failure, disease progression and fibrosis were the most common mechanisms.
Re-repair was performed for a larger share of early repair failures (40%) than late repair failures (24%). Shorter time to reoperation was the factor most strongly associated with re-repair in multivariable analysis: median time from to reoperation was 1.3 years for patients undergoing re-repair versus 3.9 years for those undergoing valve replacement. Moreover, the later in the study period a reoperation took place, the likelier it was to be a re-repair rather than a valve replacement.
Advertisement
“Over the last five years of the study, we saw a trend toward more aggressive use of re-repair,” Dr. Gillinov notes. “More than 90% of those re-repairs were done for annuloplasty dehiscence, systolic anterior motion and adverse ventricular remodeling. Mitral valve replacement was still performed for patients with progressive fibrosis or mitral stenosis.”
Compared with the replacement group, patients who underwent re-repair were younger, had fewer preexisting cardiac and noncardiac comorbidities, and were less likely to have advanced New York Heart Association symptoms. They also were less likely to undergo concomitant cardiac procedures.
No hospital deaths occurred in patients who underwent re-repair; two patients who underwent valve replacement died (0.8%). At seven years after reoperation, freedom from severe MR was 93% in the re-repair group and freedom from reoperation was 86%. Unadjusted survival after mitral reoperation was 91% at one year, 77% at five years and 59% at 10 years across the entire cohort, with similar rates between the re-repair and replacement groups. Long-term survival after re-repair was comparable to that of the age- and sex-matched general U.S. population.
Based on their results, the authors theorize that early mitral valve repair failures may be more readily repairable because relatively straightforward technical factors often are implicated, whereas late failures tend to involve reactive changes such as fibrosis and leaflet scarring.
When weighing whether to perform re-repair or replacement, they advise surgeons to consider the benefits of repair, which include freedom from anticoagulation therapy, lower risk of endocarditis and better preservation of left ventricular function.
Advertisement
Age and advanced comorbidities also need to be part of decision-making, Dr. Gillinov notes. His bottom-line advice to colleagues is to selectively employ re-repair when it is clear why a patient’s original repair failed and the pathology allows confidence that an excellent result can be achieved.
“Our recent experience supports greater applicability of re-repair than has been reported previously,” he concludes. “At Cleveland Clinic, we will continue our intentional efforts to repair as many mitral valves as possible based on growing evidence that repair offers significant advantages overall, even in reoperative settings.”
“Mitral valve repair is the optimal therapy for severe MR related to mitral valve prolapse because of the survival advantage compared with valve replacement or medical therapy,” adds Brian Griffin, MD, Medical Director of Cleveland Clinic’s Mitral and Tricuspid Valve Center. “It’s great to see that in the relatively unusual event of early failure of the repair, re-repair is often feasible and has excellent long-term outcomes as well.”
Advertisement
Advertisement
NIH-funded comparative trial will complete enrollment soon
Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic
Why and how Cleveland Clinic achieves repair in 99% of patients
Two surgeons share insights on weighing considerations across the lifespan
An overview of growth in robot-assisted surgery, impressive re-repair success rates and more
Judicious application yields a 99.7% repair rate and 0.04% mortality
A call for surgical guidelines to adopt sex-specific thresholds of LV size and function
Cleveland Clinic series shows re-repair is feasible with excellent midterm results