An updated review of risk factors, management and treatment considerations
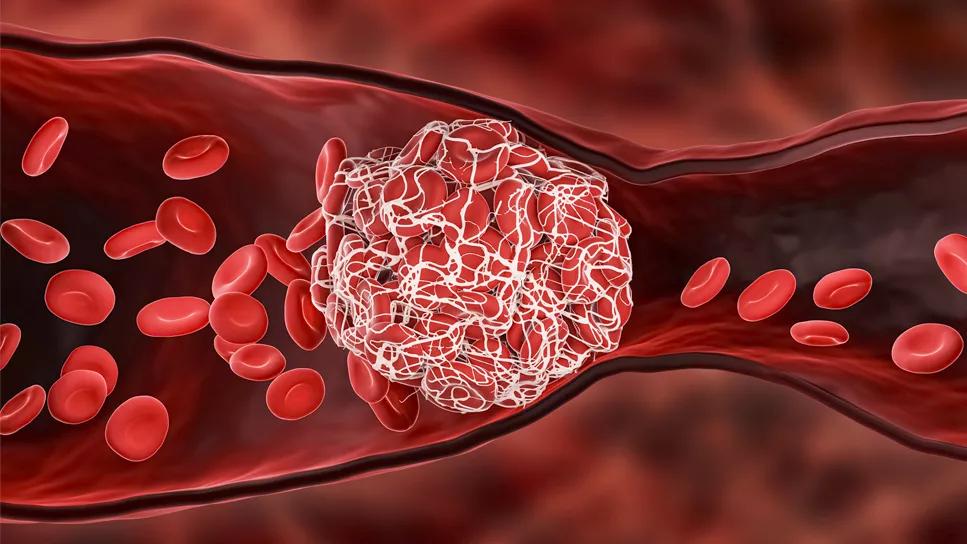
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/25a3ec79-7f7f-4783-b40f-add6d8bf6308/venous-thromboembolism-5029408)
medical illustration of thrombosis
This article was republished from the Cleveland Clinic Journal of Medicine April 2024, 91 (4) 229-235.
Farah Ziyadeh, MD and Yael Mauer, MD, MPH
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Treatment of venous thromboembolism (VTE), including deep vein thrombosis (DVT), depends on a variety of factors. The location of the VTE, severity of symptoms, risk of extension of thrombus, bleeding risk, comorbidities, and patient preferences affect the decision to treat, the choice of antithrombotic agent, and the duration of therapy, as outlined in the 2021 updated guidelines of the American College of Chest Physicians (CHEST).1
In patients with isolated distal DVT (below the popliteal vein) without high-risk features, monitoring progression is recommended over starting anticoagulation. However, it is strongly recommended to treat proximal DVT with anti-coagulation. More evidence now supports the treatment of superficial vein thrombosis with anticoagulation in high-risk patients.1
In this article, we review risk factors, supportive management, choice of anticoagulation therapy, and treatment considerations in special patient populations.
According to the U.S. Centers for Disease Control and Prevention (CDC), approximately 900,000 people in the United States are affected by VTE each year, and 3 out of 10 will have recurrence of a clotting event within 10 years.2 The prevalence of distal DVT, which varies widely because of different patient populations and diagnostic strategies used in studies, ranges from 23% to 59% in patients who received a diagnosis of DVT.3
In a population-based study, the most common risk factors for VTE included limited mobility for more than 48 hours in the past 30 days (defined as, at most, from bed to chair or bathroom), recent or current hospitalization, recent surgery, recent infection, and active malignancy.4 The annual diagnosis rate for lower-extremity superficial vein thrombosis (SVT) was 0.64% in a prospective study.5 The diagnosis rate increased with age, and SVT was more common in women. Patients at greater risk of developing SVT include women older than age 60 and individuals with obesity, pregnancy, smoking, infection, chronic venous insufficiency, and varicose veins.5
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/550857ca-833c-4ec1-a0aa-f4c0fe2e49cf/thrombosis-chart-inset)
Isolated distal DVT (“calf DVT”) is VTE below the popliteal vein.6 The 2021 CHEST guidelines1 recommend anticoagulation for at least three months for patients with a high risk of thrombus extension (Table)1,7–9, as these patients are at greater risk of progression to proximal DVT and pulmonary embolism.1
In contrast, patients with a low risk of thrombus extension (i.e., they do not meet the criteria in the table) should be monitored for extension with serial ultrasonography once weekly for two weeks, as well as for worsening of symptoms.1 However, this is a weak recommendation with moderate-certainty evidence.1 In patients for whom the inconvenience of weekly imaging out weighs the potential bleeding risk, anticoagulation for three months is a reasonable alternative.1
When the decision is to monitor with serial duplex venous ultrasonography, patients without extension of the thrombus require no anticoagulation, a strong recommendation with moderate-certainty evidence.1 Proximal propagation (to the popliteal vein or higher) occurs in 8% to 15% of cases of isolated distal DVT followed with duplex ultrasonography surveillance.10 For patients with evidence of proximal extension, there is a strong recommendation to anticoagulate for three months.1
A retrospective study showed that nine of 212 patients monitored with Doppler ultrasonography had new DVT in a distal branch of the original lesion.7 For extension confined to distal veins or for new distal thrombosis, the recommendation is to anticoagulate for three months, but this is a weak recommendation with a very low certainty of evidence.1
Advertisement
Proximal DVT is defined as thrombus in the popliteal, femoral or iliac veins.7,11 The 2021 CHEST guidelines recommend treating proximal DVT with anticoagulation for at least three months.1,6 Proximal DVT confers up to a 50% risk of pulmonary embolism if left untreated,12 so treatment with anticoagulation is recommended even in the absence of symptoms (incidental DVT).1,11
Use of an inferior vena cava filter should be considered only in patients deemed to have an unacceptably high bleeding risk.1,8,11,13,14 Because the filters confer significant risk (occlusion, inferior vena cava strut penetration, filter embolization, movement or fracture, and complications of insertion), it should be removed as soon as possible after anticoagulation is resumed.1,13
SVT is defined as thrombus involving superficial veins of the upper or lower extremities.15 The 2021 CHEST guidelines recommend treatment of patients with SVT having high-risk features1,15,16 with 45 days of anticoagulation (weak recommendation based on moderate-certainty evidence).1 Patients with SVT and high-risk features should also be screened for DVT with bilateral ultrasonography due to the high likelihood of undiagnosed DVT.15 Patients with SVT who do not have high-risk features do not require additional treatment with anti-coagulation or screening for DVT. Anticoagulant therapy is generally not recommended to treat SVT associated with intravenous therapy.1
It is important to note that patients with DVT and SVT should be screened for signs and symptoms of pulmonary embolism because of the risk of progression from SVT to DVT and subsequently to pulmonary embolism.15 One study reported concomitant symptomatic pulmonary embolism in 4.7% of patients with SVT at the time of presentation.5 Another study reported concomitant pulmonary embolism in approximately half of patients with DVT.17
Advertisement
Post-thrombotic syndrome is a common complication of lower-extremity DVT, reported in 20% to 50% of patients after proximal DVT.18,19 Previous CHEST guidelines had recommended the use of compression stockings in patients with DVT to reduce the likelihood of developing post-thrombotic syndrome.11 However, the 2021 CHEST guidelines and the 2023 National Institute for Health and Care Excellence guidelines20 no longer recommend this practice.
Oral anticoagulants used in the treatment of VTE include the direct oral anticoagulants (DOACs) apixaban, rivaroxaban, edoxaban and dabigatran, and the vitamin K antagonist warfarin. Parenteral options include low-molecular-weight heparin (LMWH) and fondaparinux. The choice of agent depends on comorbidities, renal and liver function, risk of bleeding, affordability and patient preferences.11,21–24
DOACs offer a predictable anticoagulation effect with fixed dosing and do not require laboratory monitoring.21 However, they should be used with caution in patients with renal and hepatic dysfunction. They are also significantly more expensive than warfarin.25
Warfarin requires frequent laboratory monitoring and dosing adjustments to ensure that the international normalized ratio is within therapeutic range. It also has many drug-drug interactions, requires dietary restrictions, causes fluctuations in the international normalized ratio, and can increase the risk of bleeding or recurrent thrombosis, as well as first events in patients taking it for other indications such as atrial fibrillation.21,22
Advertisement
The 2021 CHEST guidelines recommend the use of DOACs over warfarin whenever possible, based on data showing a lower risk of major bleeding (especially intracranial hemorrhage) with DOACs versus warfarin (strong recommendation with moderate-certainty evidence).1,21
The 2021 CHEST guidelines recommend fondaparinux as the agent of choice for the treatment of SVT, but rivaroxaban is an acceptable alternative.1,24 A randomized trial showed that fondaparinux was associated with a lower incidence of SVT extension compared with placebo in patients with acute symptomatic SVT of the legs.26 The SURPRISE trial (Superficial Vein thrombosis Treated for Forty-five Days With Rivaroxaban Versus Fondaparinux) found rivaroxaban to be noninferior to fondaparinux for the treatment of SVT in terms of development of symptomatic DVT or pulmonary embolism, progression or recurrence of SVT, and all-cause mortality, and was not associated with more major bleeding.24
Patients with cancer have a markedly increased risk of thromboembolism and bleeding.27,28 In patients with cancer-associated VTE, oral factor Xa inhibitors (apixaban, edoxaban, rivaroxaban) are recommended over LMWH or vitamin K antagonists because of the oral administration of DOACs and their safety and efficacy without the need for laboratory monitoring.1 In a recent meta-analysis of patients with cancer-associated VTE, oral factor Xa inhibitors reduced the risk of recurrent VTE similarly to LMWH, without a significantly higher likelihood of major bleeding.27
Patients with gastrointestinal and genitourinary malignancies may constitute an exception to the above recommendation, as there is an increased risk of bleeding in these patients with use of rivaroxaban and edoxaban when compared with LMWH,29–31 but apixaban seems to be noninferior to LMWH, with no increased risk of major bleeding.1,30 Thus, apixaban or LMWH is recommended in patients with high risk for mucosal bleeding.1,30 Vitamin K antagonists are not favored in patients with cancer-associated thrombosis given the moderate-certainty evidence that LMWH is more effective in reducing recurrence of VTE, as well as the difficulty with maintaining a therapeutic range. In addition, LMWH would be easier to withhold or adjust than vitamin K antagonists for invasive interventions, if needed.1
Patients with antiphospholipid syndrome are at increased risk of VTE as well as arterial thrombosis.32 The use of DOACs to treat VTE in antiphospholipid syndrome is not well studied, but emerging data suggest a higher risk of arterial thrombosis with DOACs than with vitamin K antagonists.32 Current recommendations favor the use of vitamin K antagonists over DOACs for VTE treatment in these patients, especially those with triple-positive antiphospholipid syndrome (presence of lupus anticoagulant, anticardiolipin, and anti-beta-2-glycoprotein 1 antibodies).1,33 If patients experience a thrombotic event while on a therapeutic dose of warfarin, treatment options include increasing the target international normalized ratio, LMWH, and fondaparinux, or the addition of an antiplatelet agent.1
When anticoagulation is indicated in patients with DVT, treatment should continue for at least three months after the initial thrombotic episode.1 Anticoagulation beyond three months, without a specific end date, is recommended for patients at particularly high risk of recurrence or for those with a history of prior VTE. Regardless of initial risk factors, a reassessment of risk for VTE recurrence, risk of bleeding, and patient preferences should be pursued annually and at times of significant changes in health status.1 For extended anticoagulation, a reduced dose of apixaban or rivaroxaban is recommended (weak recommendation with a very low certainty of evidence).
1. Stevens SM, Woller SC, Kreuziger LB, et al. Antithrombotic therapy for VTE disease: second update of the CHEST Guideline and Expert Panel report [published correction appears in Chest 2022; 162(1):269]. Chest 2021; 160(6):e545–e608.
2. U.S. Centers for Disease Control and Prevention. Data and statistics on venous thromboembolism. Updated June 28, 2023. www.cdc.gov/ncbddd/dvt/data.html. Accessed March 12, 2024.
3. Palareti G. How I treat isolated distal deep vein thrombosis (IDDVT). Blood 2014; 123(12):1802–1809.
4. Spencer FA, Emery C, Lessard D, et al. The Worcester Venous Thromboembolism Study: a population-based study of the clinical epidemiology of venous thromboembolism. J Gen Intern Med 2006; 21(7):722–727.
5. Frappé P, Buchmuller-Cordier A, Bertoletti L, et al. Annual diagnosis rate of superficial vein thrombosis of the lower limbs: the STEPH community-based study [published correction appears in J Thromb Haemost 2015; 13(8):1538]. J Thromb Haemost 2014; 12(6):831–838.
6. Robert-Ebadi H, Righini M. Management of distal deep vein thrombosis. Thromb Res 2017; 149:48–55.
7. Fujioka S, Ohkubo H, Kitamura T, et al. Risk factors for progression of distal deep vein thrombosis. Circ J 2020; 84(10):1862–1865.
8. Nieto JA, Solano R, Ruiz-Ribó MD, et al. Fatal bleeding in patients receiving anticoagulant therapy for venous thromboembolism: findings from the RIETE registry. J Thromb Haemost 2010; 8(6):1216–1222.
9. Sartori M, Favaretto E, Cosmi B. Relevance of immobility as a risk factor for symptomatic proximal and isolated distal deep vein thrombosis in acutely ill medical inpatients. Vasc Med 2021; 26(5):542–548.
10. Masuda EM, Kistner RL. The case for managing calf vein thrombi with duplex surveillance and selective anticoagulation. Dis Mon 2010; 56(10):601–613.
11. Kearon C, Akl EA, Comerota AJ, et al. Antithrombotic therapy for VTE disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines [published correction appears in Chest 2012; 142(6):1698–1704]. Chest 2012; 141(2 suppl):e419S–e496S.
12. Kearon C. Natural history of venous thromboembolism. Circulation 2003; 107(23 suppl 1):I22–I30. doi:10.1161/01.CIR.0000078464.82671.78
13. Duffett L, Carrier M. Inferior vena cava filters. J Thromb Haemost 2017; 15(1):3–12.
14. DeYoung E, Minocha J. Inferior vena cava filters: guidelines, best practice, and expanding indications. Semin Intervent Radiol 2016; 33(2):65–70.
15. Beyer-Westendorf J. Controversies in venous thromboembolism: to treat or not to treat superficial vein thrombosis. Hematology Am Soc Hematol Educ Program 2017; 2017(1):223–230.
16. Leizorovicz A, Becker F, Buchmüller A, et al. Clinical relevance of symptomatic superficial-vein thrombosis extension: lessons from the CALISTO study. Blood 2013; 122(10):1724–1729.
17. Lee JS, Moon T, Kim TH, et al. Deep vein thrombosis in patients with pulmonary embolism: prevalence, clinical significance and outcome. Vasc Specialist Int 2016; 32(4):166–174.
18. Galanaud JP, Monreal M, Kahn SR. Epidemiology of the post-thrombotic syndrome. Thromb Res 2018; 164:100–109.
19. Appelen D, van Loo E, Prins MH, Neumann MH, Kolbach DN. Compression therapy for prevention of post-thrombotic syndrome. Cochrane Database Syst Rev 2017; 9(9):CD004174.
20. National Institute for Health and Care Excellence (NICE). Venous thromboembolic diseases: diagnosis, management and thrombophilia testing. London: National Institute for Health and Care Excellence (NICE); August 2, 2023. https://www.ncbi.nlm.nih.gov/ books/NBK556698/. Accessed March 12, 2024.
21. Yeh CH, Gross PL, Weitz JI. Evolving use of new oral anticoagulants for treatment of venous thromboembolism. Blood 2014; 124(7):1020–1028.
22. Witt DM, Nieuwlaat R, Clark NP, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: optimal management of anticoagulation therapy. Blood Adv 2018; 2(22):3257–3291.
23. GoodRx, Inc. Stop paying too much for prescriptions. www.goodrx. com. Accessed March 12, 2024.
24. Beyer-Westendorf J, Schellong SM, Gerlach H, et al. Prevention of thromboembolic complications in patients with superficial-vein thrombosis given rivaroxaban or fondaparinux: the open-label, randomised, non-inferiority SURPRISE phase 3b trial. Lancet Haematol 2017; 4(3):e105–e113.
25. Ortel TL, Neumann I, Ageno W, et al. American Society of Hematology 2020 guidelines for management of venous thromboembolism: treatment of deep vein thrombosis and pulmonary embolism. Blood Adv 2020; 4(19):4693–4738.
26. Decousus H, Prandoni P, Mismetti P, et al. Fondaparinux for the treatment of superficial-vein thrombosis in the legs. N Engl J Med 2010; 363(13):1222–1232.
27. Wang X, Ma Y, Hui X, et al. Oral direct thrombin inhibitors or oral factor Xa inhibitors versus conventional anticoagulants for the treatment of deep vein thrombosis. Cochrane Database Syst Rev 2023; 4(4):CD010956.
28. Prandoni P, Lensing AW, Piccioli A, et al. Recurrent venous thromboembolism and bleeding complications during anticoagulant treatment in patients with cancer and venous thrombosis. Blood 2002; 100(10):3484–3488.
29. Key NS, Khorana AA, Kuderer NM, et al. Venous thromboembolism prophylaxis and treatment in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol 2020; 38(5):496–520.
30. Agnelli G, Becattini C, Meyer G, et al. Apixaban for the treatment of venous thromboembolism associated with cancer. N Engl J Med 2020; 382(17):1599–1607.
31. Raskob GE, van Es N, Verhamme P, et al. Edoxaban for the treatment of cancer-associated venous thromboembolism. N Engl J Med 2018; 378(7):615–624.
32. Woller SC, Stevens SM, Kaplan D, et al. Apixaban compared with warfarin to prevent thrombosis in thrombotic antiphospholipid syndrome: a randomized trial. Blood Adv 2022; 6(6):1661–1670.
33. Zuily S, Cohen H, Isenberg D, et al. Use of direct oral anticoagulants in patients with thrombotic antiphospholipid syndrome: guidance from the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. J Thromb Haemost 2020; 18(9):2126–2137.
34. Kearon C, Ageno W, Cannegieter SC, et al. Categorization of patients as having provoked or unprovoked venous thromboembolism: guidance from the SSC of ISTH. J Thromb Haemost 2016; 14(7):1480–1483.
Advertisement
Oral anticoagulants may be beneficial but need to be balanced against bleeding risks
Redesigned protocols enhance infection-prevention measures
Patients with a prior history of VTA are at an increased risk of subsequent incidents, despite treatment with therapeutic anticoagulation
Findings help close the knowledge gap around VTE practice patterns
Novel approach outperforms standard of care for post-PVI stenosis and occlusion
Data from combined prospective and retrospective cohorts support the drug’s safety and efficacy for CLVM
Clinicians highlight the need to educate patients about warning signs
Emerging evidence suggests a patient-specific approach