Clinical trial to investigate pain management for head and neck cancer patients
A new clinical trial will soon be underway at Cleveland Clinic to examine the effects of a perioperative, multimodal, non-opioid analgesia regimen in head and neck cancer patients. The goal is to effectively manage and standardize pain control throughout the perioperative period for a population undergoing among the most complex head and neck surgeries – namely, those with microvascular free flap reconstruction.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The opioid epidemic in the United States has catalyzed efforts to reexamine practices in pain management and regulate its use. In addition, limiting opioids in postsurgical care can serve to decrease common side effects such as nausea and constipation. This poses a unique challenge to head and neck surgical oncologists whose patients are susceptible to significant perioperative pain. In addition to increased pain sensitivity associated with the neuroanatomy of the head and neck, many patients undergoing treatment require multiple surgical sites, which may contribute to increased postoperative discomfort.
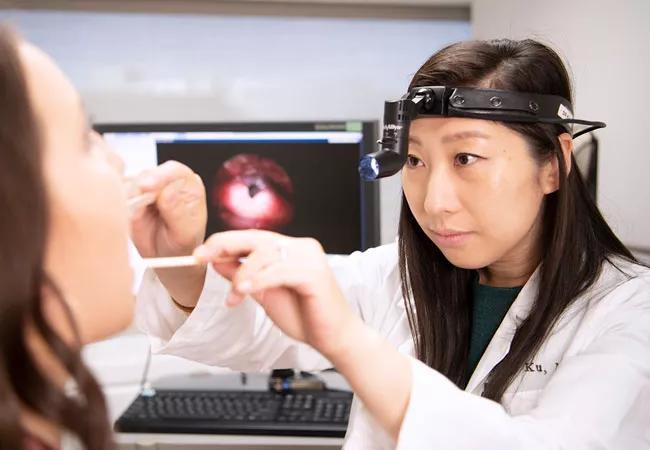
Jamie Ku, MD, principal investigator of the study and head and neck surgical oncologist and microvascular reconstructive surgeon in Cleveland Clinic’s Head & Neck Institute, hopes the study will bring new insights to pain control for patients undergoing surgery for head and neck cancers. “We want to standardize protocols for head and neck surgery patients and, at the same time, identify an effective medication regimen that can minimize reliance on opioids,” says Dr. Ku.
The randomized, double-blind, placebo-controlled trial will examine a combination of acetaminophen, celecoxib, gabapentin, lidocaine and ketamine at 48- and 96-hour intervals following surgery. The investigators hypothesize that the perioperative analgesics, both cost-effective and accessible, will lead to lower reported pain scores and opioid consumption while decreasing opioid-related side effects and increasing patient satisfaction. As a secondary benefit, this approach may also decrease a patient’s length of hospital stay, readmission rate, overall cost-of-care and chronic pain.
Advertisement
Other studies have investigated non-opiate regimens in head and neck surgery patient populations, but the literature is largely retrospective. Few studies have conducted a prospective analysis. This trial may establish a foundation for such investigations in the future. “At this point, we aren’t trying to determine which one specific medicine is contributing to a potential difference but studying the effect of the entire regimen as a whole,” she says. The current goal is to validate whether the perioperative, multimodal analgesic approach offers an improved clinical value versus the placebo.
She also points out that a shift to non-opiate alternatives is more than just a change in the clinical management of patients. “This means managing patient and clinician expectations about postoperative pain management in a new way.”
This, evidenced by a recent study that found a significantly lower frequency of postoperative opioid use in an international head and neck surgical program compared to a domestic one. These expectations and behaviors are often rooted in social and cultural norms, says Dr. Ku. “Non-opiate alternatives have, historically, not been a significant part of practice in the U.S.”
“Though this work is focused on a specific, albeit vulnerable patient population, our hope is that findings will contribute to a larger conversation in healthcare about rethinking pain protocols and improving postoperative care for all patients.”
Funding for this project was made possible by a VeloSano Pilot Award, which recognizes some of the most promising cancer research projects at Cleveland Clinic.
Advertisement
Advertisement

Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor

Case study illustrates the potential of a dual-subspecialist approach

Evidence-based recommendations for balancing cancer control with quality of life

Study shows no negative impact for individuals with better contralateral ear performance

HNS device offers new solution for those struggling with CPAP

Patient with cerebral palsy undergoes life-saving tumor resection

Specialists are increasingly relying on otolaryngologists for evaluation and treatment of the complex condition

Detailed surgical process uncovers extensive middle ear damage causing severe pain and pressure.