True for temporal artery, biopsy neg/pos GCA
Researchers have long suspected that microorganisms play a role in the development of giant cell arteritis (GCA); data showing that patients with the disease have a distinct microbiome are the first step toward determining that function.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
GCA occurs most often in the extracranial branches of the carotid arteries near the temple and is the most common large vessel vasculitis. Evidence suggests that infectious agents may provide antigenic stimulation in GCA. With this in mind, researchers recently analyzed bacterial sequences and abundance in patients with GCA and compared them with patients without GCA.
“The etiology of GCA is unknown, but the immunologic features of the disease suggest that microorganisms may play a role,” says Alexandra Villa-Forte, MD, MPH, staff in the Department of Rheumatic and Immunologic Diseases and an author on the paper published in Pathogens and Immunity. “However, a distinct vascular microbial environment could also be a secondary result stemming from injury to the vessel itself.”
The study authors enrolled 47 patients. Patients with GCA were a median age of 71 at the time of biopsy; median age was 73 for non-GCA controls. Of 47 patients, 74% had been receiving daily prednisone (mean dose > 50mg/day) before their temporal artery biopsies (89% in the GCA biopsy-positive group, 86% of GCA biopsy-negative patients and 71% of controls).
The researchers classified the patients as either biopsy-positive GCA (nine patients), biopsy-negative GCA (15 patients) or as controls (23 patients). Patients’ baseline characteristics included corticosteroid use, clinical symptoms, laboratory markers, comorbidities and histopathology.
A team of ophthalmologists collected the biopsies under strictly aseptic conditions, then split them, with half sent for routine histopathological review and half snap-frozen under sterile technique for microbiome analysis. Following more than three years of collection, all samples were processed at the same time. Laboratory-based microbiome investigators did not know the patients’ clinical and pathological diagnoses.
Advertisement
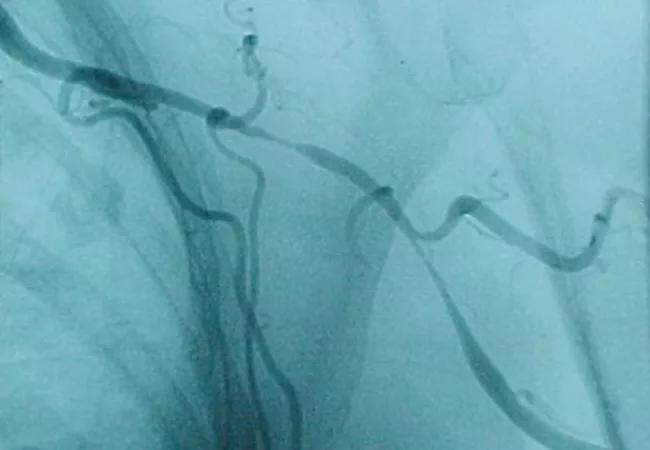
Histopathology of temporal artery of the nine patients with a final diagnosis of biopsy-proven GCA revealed arteritis, with mononuclear cell inflammatory infiltrates localized to the media and adventitia, varying amounts of intimal proliferation and fibrinoid necrosis, and fragmentation of the internal elastic lamina.
All biopsies from biopsy-negative patients with clinically positive GCA, revealed arteriosclerosis, with intimal thickening and rare, focal calcification; 20 of 23 control TA without GCA also shared these findings. Tthree TA from controls were normal.
FISH showed multiple single bacteria in the media of both control and GCA-involved temporal arteries. FISH signal corresponding to the presence of bacteria was not seen in the arterial lumen, intimal layer or external border of the specimens. Aligning with the FISH microscopy, the mean intensity for the FISH-positive bacteria was higher in GCA-involved arteries compared with that of the control. There was no signal ascertained at a GCA-involved temporal artery’s external edge.
The investigators compared the relative abundances of bacterial operational taxonomic units in temporal arteries of patients with and without GCA. At least two classes of Firmicutes were relatively over-represented at the phylum level in GCA temporal arteries compared with those without GCA. Two other classes of Firmicutes were relatively under-represented in temporal arteries with GCA compared with temporal arteries without GCA.
In TA samples from patients with GCA, Proteobacteria and Actinobacteria were relatively under-represented. At the genus level, Granulicatella and Streptococcus in phylum Firmicutes were relatively over-represented. Parasutterella, in phylum Proteobacteria, and Bifidobacterium, in phylum Actinobacteria, were relatively under-represented in TA samples from patients with GCA.
Advertisement
“Overall, we learned that temporal arteries are not sterile, as previously assumed, but rather are inhabited by communities of bacteria in both the control and diseased states,” says Charis Eng, MD, PhD, Chair of Cleveland Clinic’s Genomic Medicine Institute. “We also found that the microbiomes of biopsy-negative, clinically confirmed GCA temporal arteries were similar to those of biopsy-positive GCA temporal arteries, and together these two groups were distinct from those in control group samples. All of this leads us to wonder why there are histopathologic differences between biopsy-positive and biopsy-negative individuals with GCA.”
One idea is that microbiomes may play a permissive role in the pathogenesis of GCA, to be later followed by a histologically apparent inflammatory response. If this were true, the well-known “skip lesions” in GCA biopsies could result from a stepwise inflammatory response.
Advertisement
Advertisement

The case for continued vigilance, counseling and antivirals

High fevers, diffuse rashes pointed to an unexpected diagnosis

No-cost learning and CME credit are part of this webcast series

Summit broadens understanding of new therapies and disease management

Program empowers users with PsA to take charge of their mental well being

Nitric oxide plays a key role in vascular physiology

CAR T-cell therapy may offer reason for optimism that those with SLE can experience improvement in quality of life.

Unraveling the TNFA receptor 2/dendritic cell axis