Anatomical modeling can identify optimal surgical candidates, study suggests
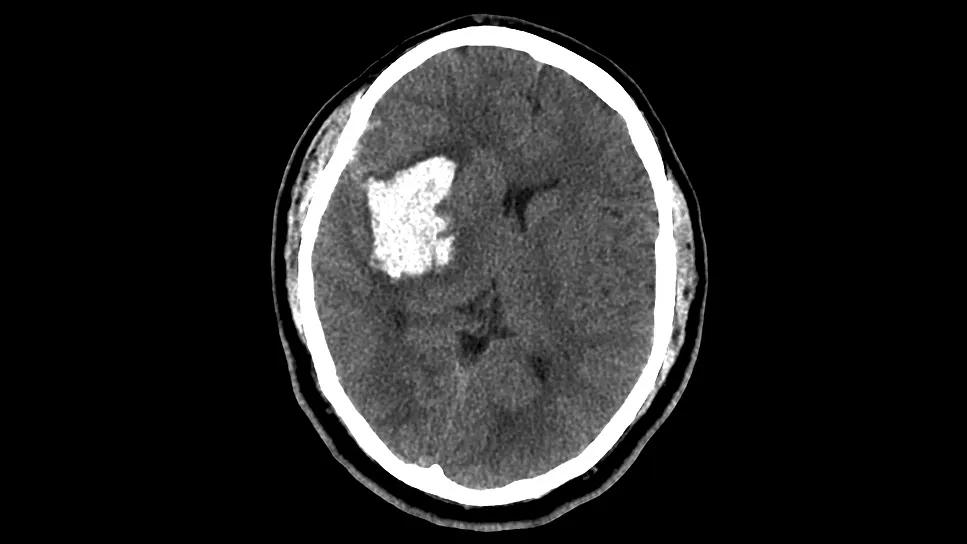
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/69af3e4a-1991-4936-b470-ac0c848cea43/mis-evacuation-for-putaminal-hemorrhage)
brain scan showing hemorrhage in the putamen
A Cleveland Clinic study focused exclusively on moderate-size putaminal intracranial hemorrhages (pICHs) has challenged previous notions about the efficacy of minimally invasive surgical (MIS) evacuation in this difficult-to-treat patient population. The findings, published in the Journal of Neurosurgery, suggest that MIS evacuation of pICHs from 10 to 50 mL in volume is associated with significantly lower one-year mortality and a shorter ICU length of stay (LOS) compared with maximal medical management.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Putaminal ICH is a subtype of basal ganglia ICH (bgICH). While prior large-scale trials have shown limited or neutral results for bgICH management, this single-center study using propensity matching provides unique insights into which patients with pICH are most likely to benefit from surgical intervention based on the hemorrhage’s precise spatial distribution. The study also introduces a method of volumetric imaging analysis, easily accessible via routine CT, that could be integrated into clinical workflows to triage management strategies and identify ideal surgical candidates.
“We believe our findings have potential to refine surgical selection criteria for patients with moderate-size putaminal hemorrhages,” says first author Ahmed Kashkoush, MD, a neurosurgery resident at Cleveland Clinic.
Although bgICH leads to death or dependence in over 70% of patients, the evidence base supporting its surgical management is highly limited. Earlier trials evaluating ICH evacuation often combined lobar and basal ganglia locations, potentially masking specific benefits in subpopulations.
As a result, surgical options for bgICH remain largely unexplored. American Heart Association (AHA) guidelines from 2022, drawing from criteria used in mixed-population trials, generally recommend considering stereotactic aspiration or MIS evacuation for ICH volumes between 20 and 30 mL in patients with moderate Glasgow Coma Scale scores. However, these guidelines do not propose specific surgical selection criteria for bgICH.
Advertisement
A key anatomical difference distinguishing bgICH from lobar ICH is the dense arrangement of highly eloquent structures, such as the internal capsule and thalamus, within a compact region. This means that the efficacy of MIS evacuation — relieving mass effect — might depend on the hemorrhage’s precise spatial orientation and its pressure on neighboring structures. Based on prior Cleveland Clinic data suggesting favorable outcomes for MIS evacuation of moderate-size pICHs (10 to 50 mL) without extensive regional spread, the authors hypothesized that MIS evacuation would improve functional outcomes compared with medical management in this specific group.
The researchers retrospectively reviewed adults admitted to Cleveland Clinic between 2013 and 2024 with spontaneous, nonlesional pICH. Inclusion required hemorrhage volumes between 10 and 50 mL, measured via volumetric CT planimetry. Exclusions included underlying structural etiologies, hemorrhagic transformation of ischemic stroke, baseline modified Rankin Scale (mRS) score > 3 and comorbidities that would prohibit surgery.
To establish equipoise, the 33 surgical patients who underwent MIS evacuation using tubular retractors were 1:1 propensity score matched to 33 medically managed patients based on ICH volume and ICH score. Medical management followed AHA recommendations, including blood pressure control and anticoagulation reversal.
The primary outcome was the utility-weighted mRS (uw-mRS) score collected within one year of hospital admission. Secondary outcomes included overall mortality, dichotomized mRS scores, ICU LOS and the incremental cost-effectiveness ratio (ICER) per quality-adjusted life year (QALY).
Advertisement
Despite the initial hypothesis focusing on improved functional outcomes, uw-mRS scores were statistically similar between the surgical and medical cohorts (mean of 0.44 and 0.33, respectively; P = .174). Rates of poor functional outcome (mRS of 4 to 6) were also statistically similar. The authors suggest that the study may have been underpowered to detect a statistical difference in functional outcomes.
However, the study showed substantial benefits in survival and resource utilization:
The authors note that a unique feature of their analysis was the use of custom stereotactic localization modeling to determine whether the hemorrhage’s spatial distribution differentially predicted outcome based on treatment strategy. This volumetric imaging analysis showed that pICH morphology did indeed influence prognosis depending on whether medical or surgical management was used, as follows:
Advertisement
While acknowledging the limitations of this study’s retrospective nature and modest sample size, the authors contend that it strongly warrants further investigation in larger, potentially multicenter studies.
“Our study provides important evidence suggesting that MIS evacuation of moderate-size putaminal ICH offers significant survival and resource utilization advantages over medical management alone,” says senior author Mark Bain, MD, MS, a Cleveland Clinic vascular neurosurgeon. “The mortality benefit observed reinforces primary findings from prior surgical studies of mixed ICH.”
He adds that the differential anatomical findings suggest that spatial distribution analysis using stereotactic localization can eventually help identify patients who are most likely to benefit from surgery. “This methodology lends itself to integration into automated computer vision platforms,” Dr. Bain concludes, “which may ultimately offer clinicians a readily available decision-making adjunct based on CT imaging.”
Advertisement
Advertisement
Ethical guidance provides guardrails so medical advances benefit patients
OCEANIC-STROKE results represent long-sought advance in secondary stroke prevention
Two studies from Cleveland Clinic may help advance the technology toward broader clinical use
Distinct MRI signature includes lesions beyond the corpus callosum, features predictive of vision and hearing loss
An argument for clarifying the nomenclature
An expert talks through the benefits, limits and unresolved questions of an evolving technology
Recommendations on identifying and managing neurodevelopmental and related challenges
Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies