Common congenital lesion is not always benign
A study underway at Cleveland Clinic aims to close gaps in the literature regarding the testing, management and long-term outcomes of patients with myocardial bridging. This common congenital lesion involves partial or complete encasement of coronary arteries, usually the left anterior descending artery (LAD), in the myocardium. The lesions vary in length and depth and were once thought to be primarily benign. More recent studies have challenged that assertion, and Cleveland Clinic’s ongoing Myocardial Bridge and Anomalous Coronary Study seeks to create a more accurate picture of how to optimally identify, evaluate and manage the condition.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“We hope our findings will get us closer to an established algorithm and guidelines for myocardial bridging,” says Joanna Ghobrial, MD, MSc, Interventional Director of Cleveland Clinic’s Adult Congenital Heart Disease Center. “Our understanding of this condition has certainly evolved from the days of assuming most cases to be benign, but now that we have more accurate tests and treatments, we need larger-scale data to guide clinicians on when and how to treat.”
The reported prevalence of myocardial bridging ranges from 1.5% to 26%, with higher numbers reported in autopsy findings versus invasive coronary angiography studies. “A good number of people are born with this condition,” notes Hani Najm, MD, Chair of Pediatric and Congenital Heart Surgery, “and yet many of them never present with symptoms, and we only find out incidentally or after death. For those who do present with symptoms, we should perform both anatomic and functional testing to determine whether they are a fit for surgery.” Symptoms can include angina, ischemia, arrhythmia, acute coronary syndrome, myocardial infarction and sudden cardiac death.
Many of those incidental findings arise from coronary CT angiography (CTA) testing, which allows for a more sophisticated view of the cardiac anatomy. “Myocardial bridges are quite common on coronary CTA,” says Paul Cremer, MD, a cardiologist in the Section of Cardiovascular Imaging. “If I see a partial encasement or superficial bridge, I usually err on the side of not commenting to discourage inappropriate downstream testing.”
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/933169cf-4f75-41b1-9c57-9c09e4928a22/20-HVI-1941483-CQD-Myocardial-Bridging-Inset-1_jpg)
Myocardial bridging is a common finding on coronary CTA. Note the partial encasement of the LAD with a distal LAD stent.
For patients with symptoms, a coronary CTA allows for more accurate assessment of the length and depth of the bridge as well as any adjacent atherosclerosis, which most often lies proximal to the bridge. “Previous studies have established coronary CTA as far superior to invasive coronary angiography in determining the anatomy of the bridging,” says Dr. Cremer. “The jury is still out on the best functional testing approach.”
Dr. Cremer presented an overview of noninvasive anatomical and functional testing in patients with myocardial bridging in a recent Tall Rounds online CME activity from Cleveland Clinic. He emphasized that functional testing should always create a hemodynamic stress, either with exercise or with dobutamine. The use of cardiac PET or MRI allows for the measurement of absolute myocardial blood flow for correlation with invasive testing.
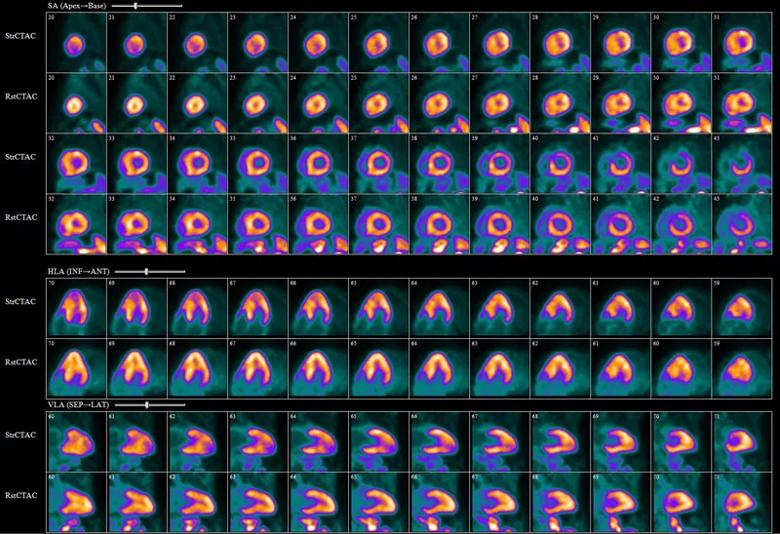
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/54522078-d443-4493-a1f8-701fe602080e/20-HVI-1941483-CQD-Myocardial-Bridging-Inset-2_jpg)
Rubidium-82 stress myocardial perfusion scan showing apical ischemia in a patient with hypertrophic cardiomyopathy. The patient underwent septal myectomy and unroofing of the mid LAD.
For symptomatic patients or those with hypertrophy or aortic stenosis, surgical intervention is sometimes recommended. “Surgery has already been established as superior to stenting, which carries a higher risk of perforation, stent fracture and thrombosis,” says Dr. Ghobrial. “Our long-term goal is that the Myocardial Bridge and Anomalous Coronary Study will supply a foundation for establishing guidelines for which patients go to surgery and when.”
Advertisement
The preferred surgical techniques are supra-arterial myotomy (unroofing) and coronary artery bypass. Bypass surgery is usually reserved for patients with longer and deeper bridges, which can extend down into the right ventricular cavity. While outcomes are fairly good, some data suggest that patients can have recurrent symptoms despite a successful procedure. “The Myocardial Bridge and Anomalous Coronary Study will give us necessary information about postsurgical unroofing success and long-term outcomes,” says Dr. Najm.
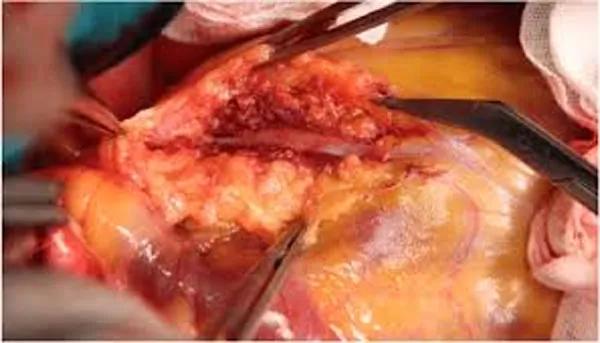
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3bde8731-c375-48bb-9033-749bd4398ff6/20-HVI-1941483-CQD-Myocardial-Bridging-Inset-3_jpg)
Supra-arterial myotomy.
Dr. Ghobrial recommends using instantaneous wave-free ratio (iFR) at rest and after dobutamine stress in the cardiac catheterization lab to functionally evaluate myocardial bridges. “We first use iFR to assess the hemodynamic effect of systolic compression from the bridging,” she says. “If there is evidence of significantly decreased perfusion during stress in symptomatic patients, we recommend surgical unroofing, and then we follow up with iFR after surgery to assess surgical success in relieving flow compromise. It’s actually quite beautiful to see the normalization of flow in these patients. We’ve had young marathon runners cleared to resume exercise, firefighters back on the job and the like.”
Cleveland Clinic uses iFR versus fractional flow reserve (FFR) to assess bridging because FFR, which gives an average of diastolic and systolic pressures, can appear normal despite significant or symptomatic bridging.
“Over the years, our experience is that most bridges look worse than their physiology indicates,” notes Cleveland Clinic interventional cardiologist Stephen Ellis, MD. “It’s important to recall that most coronary blood flow occurs in diastole when the bridge is ‘relaxed.’ Assessing physiology, one has to be careful to use a stressor appropriately mimicking the clinical condition — exercise or dobutamine, not adenosine — and to use diastolic markers of blood flow such as iFR or dPR [diastolic pressure ratio].”
Advertisement
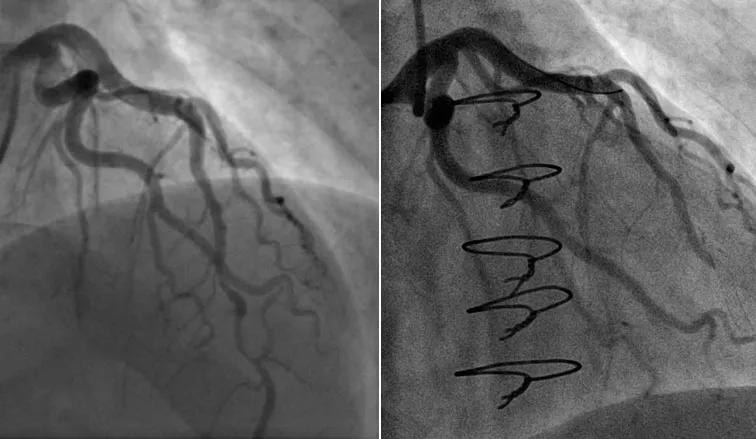
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/37823d4f-5af3-43c6-9321-f040ac5e542e/20-HVI-1941483-CQD-Myocardial-Bridging-Inset-4_jpg)
Baseline angiograms post-arrest (left) and post-unroofing (right).
While myotomy and bypass work for some patients, Cleveland Clinic also treats the most complicated myocardial bridging patients with anomalous coronary origins. “We have developed procedures here to treat patients with a transseptal course of a left main coronary artery using an autologous pericardial patch wrapped around the right ventricular outflow tract,” says Dr. Najm.
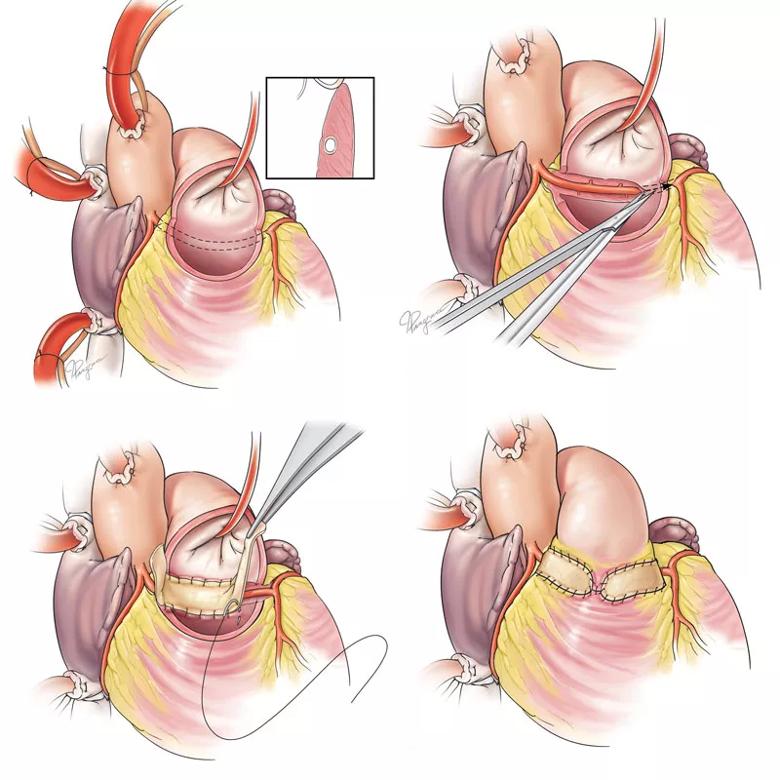
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7b081c17-0531-414b-ada5-a0d31b4f1f5a/20-HVI-1941483-CQD-Myocardial-Bridging-Inset-5_jpg)
Illustrations depicting a novel transconal approach to unroof the transseptal left main coronary artery. Top left shows the anomalous aortic origin of the left main coronary artery (AAOLCA) anatomy as viewed from inside the right ventricular outflow tract (RVOT) (inset: cross-sectional view of the coronary artery surrounded by septal muscle). Top right shows unroofing and skeletonization of the AAOLCA to the coronary bifurcation. Bottom left shows pericardial patch elongation of the posterior RVOT. Bottom right shows external view of the RVOT following pericardial patch elongation. Note that the unroofed coronary artery is posterior to the patch. Reprinted from Annals of Thoracic Surgery, vol. 108, Najm and Ahmad, “Transconal unroofing of anomalous left main coronary artery from right sinus with trans-septal course,” pages 383-386, copyright 2019, with permission from The Society of Thoracic Surgeons.
The Myocardial Bridge and Anomalous Coronary Study, led by Dr. Ghobrial, has already enrolled over 110 patients in less than two years, which is a large cohort for such a rarely symptomatic anomaly. It continues to enroll new patients, with plans to track all patients’ long-term outcomes. Researchers are optimistic that the data will bring better diagnostics and management to patients with this understudied and potentially debilitating condition.
Advertisement
Advertisement
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Cleveland Clinic’s new dedicated program offers nuanced care for a newly recognized cardiovascular risk factor
Scenarios where experience-based management nuance can matter most
Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics
How Cleveland Clinic is using and testing TMVR systems and approaches
NIH-funded comparative trial will complete enrollment soon
How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR
Optimal management requires an experienced center